Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
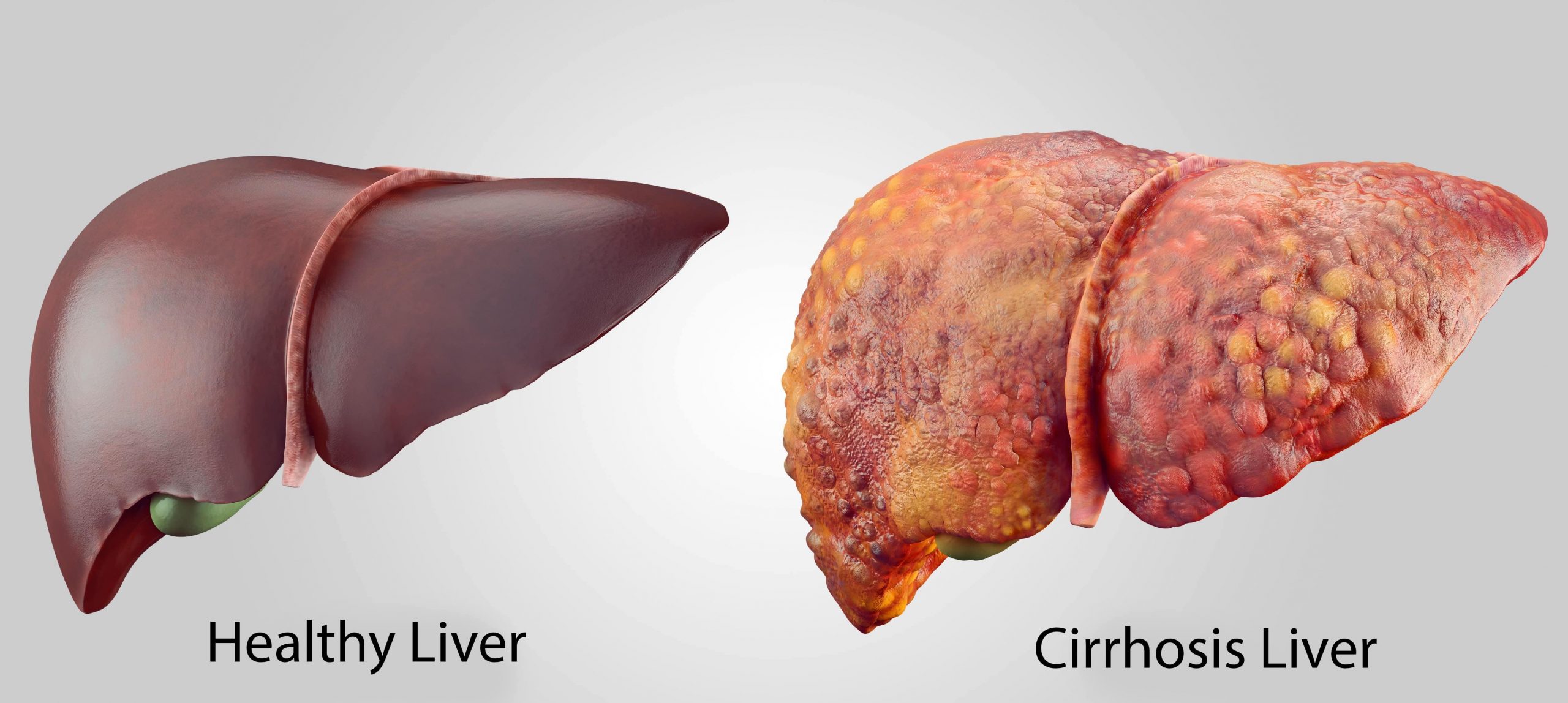
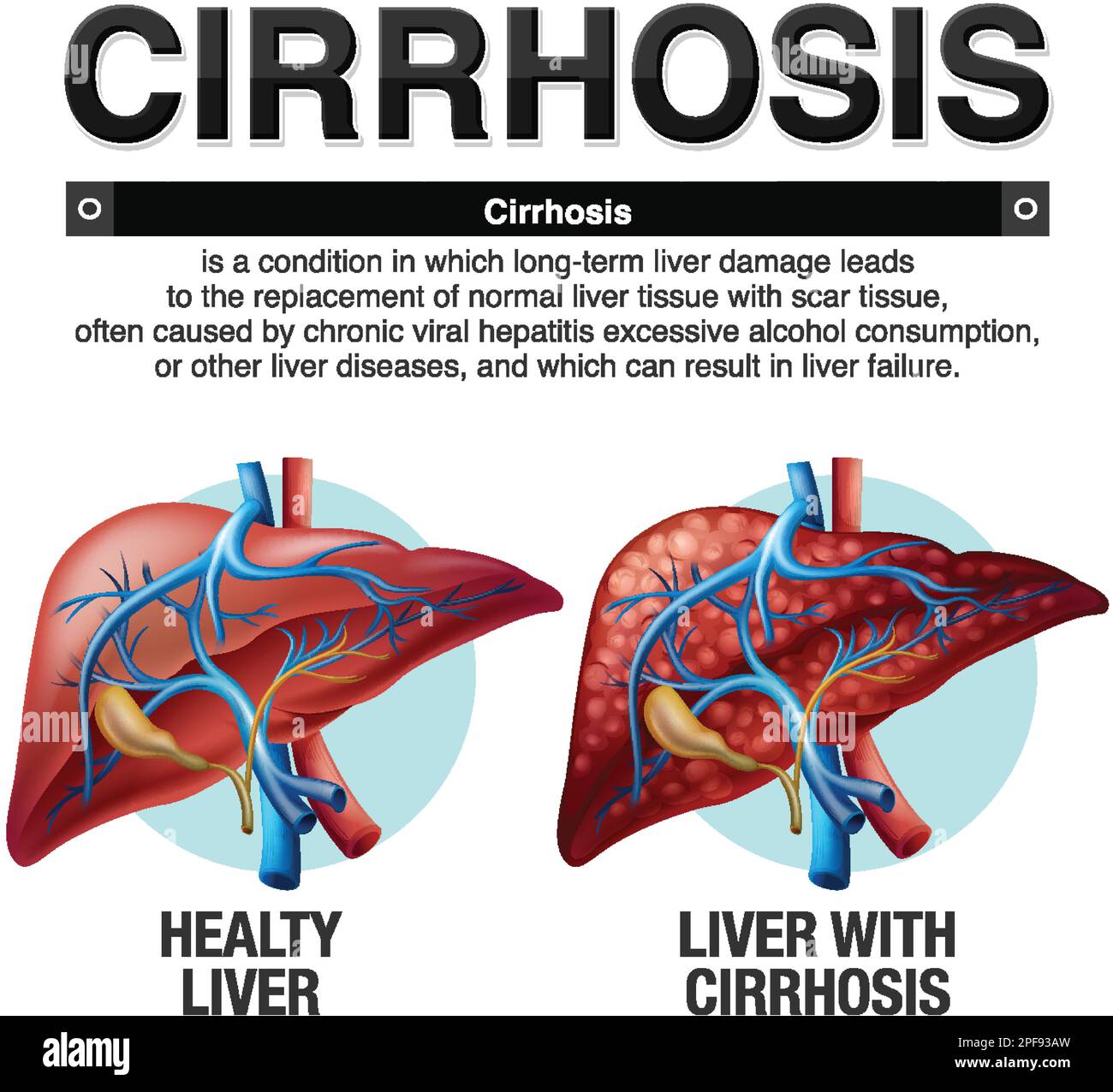
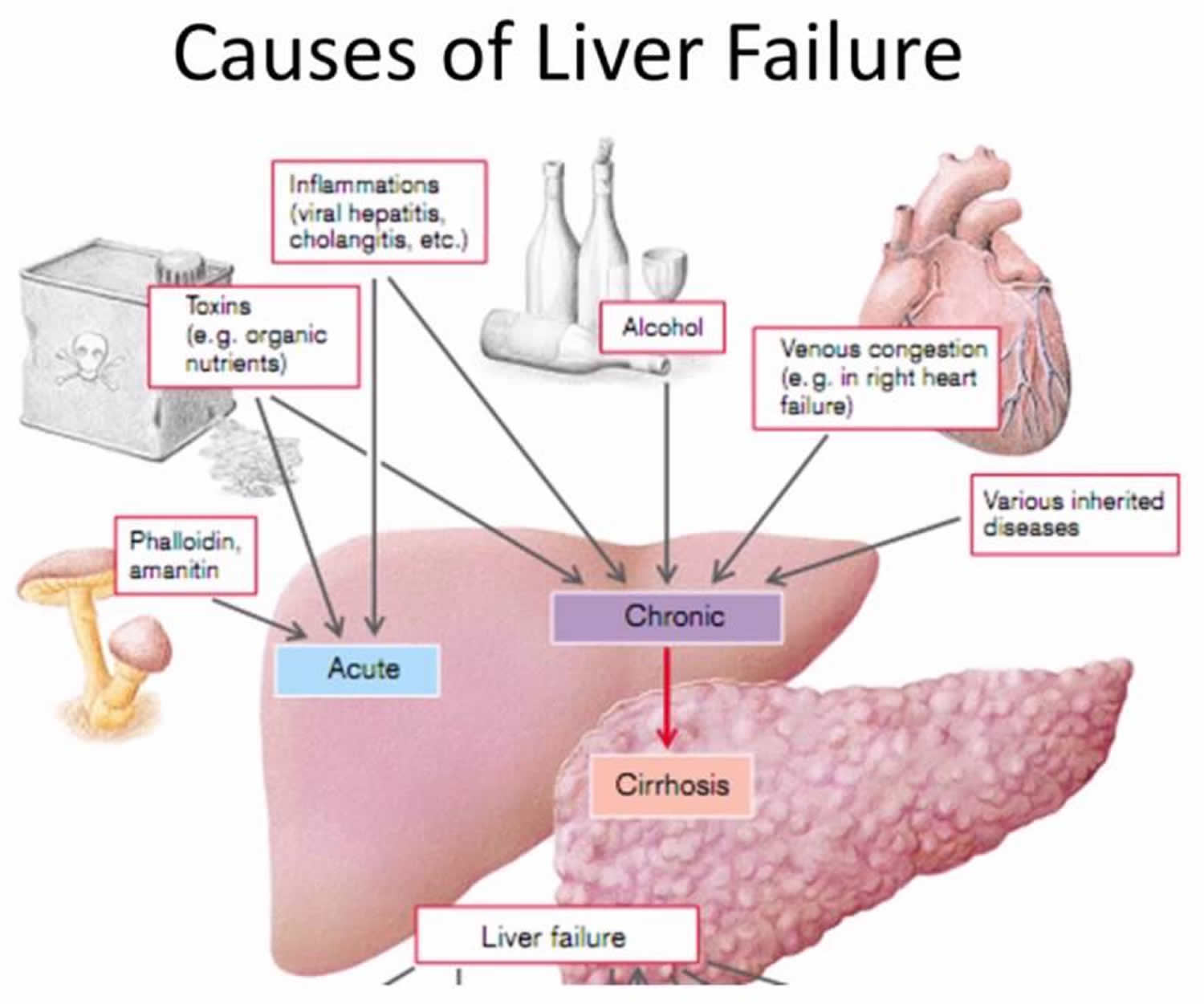
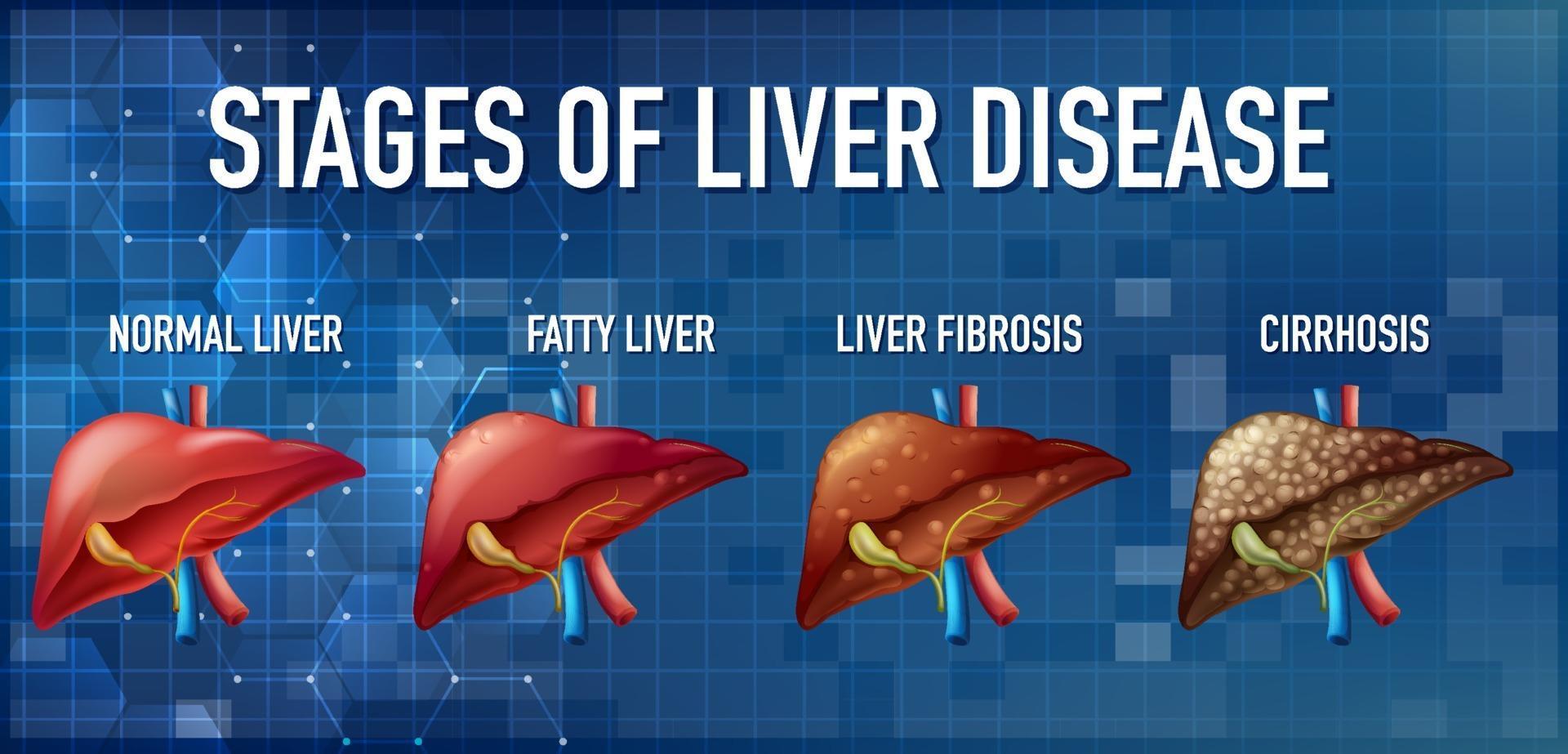
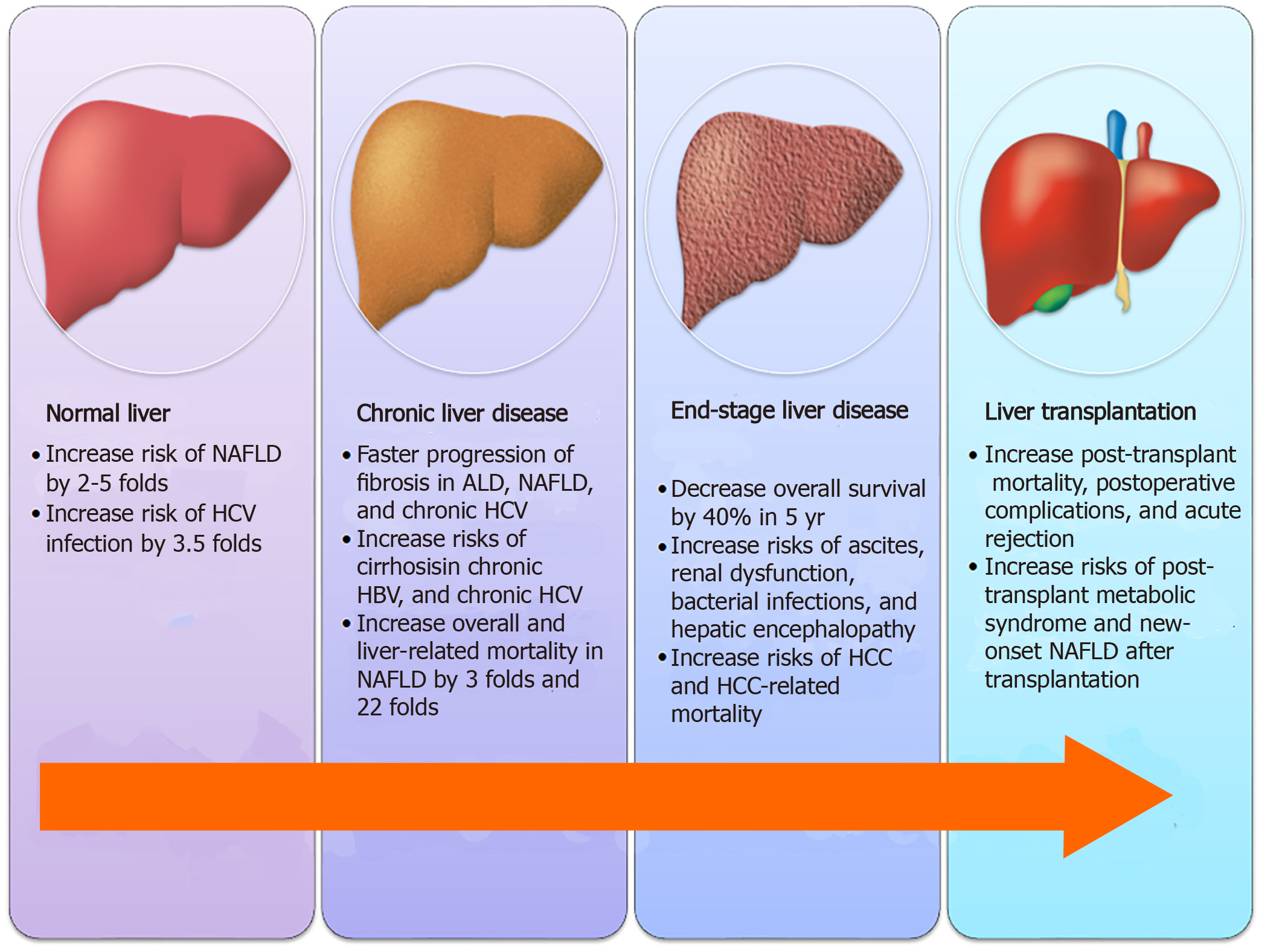
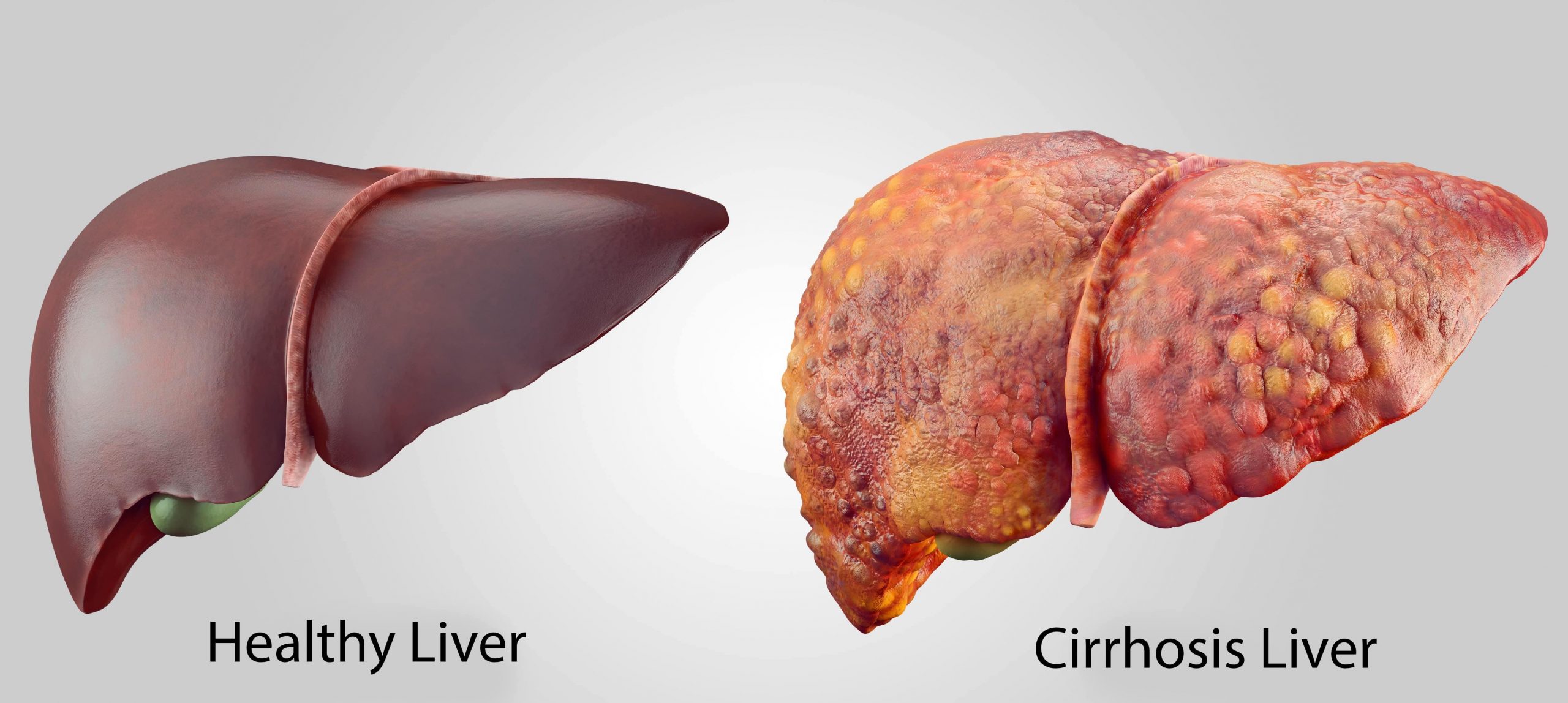
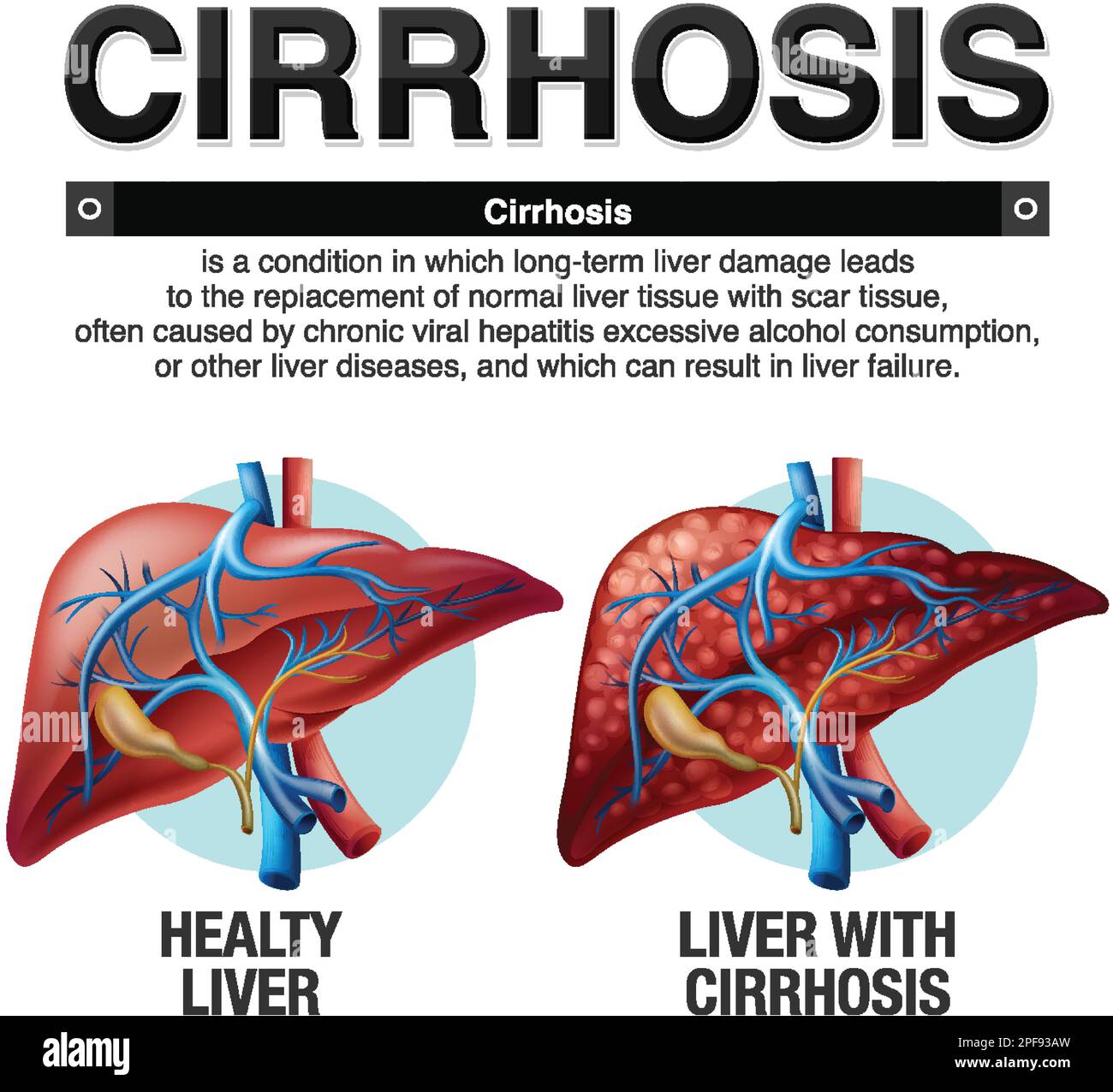
Gabapentin is a unique anticonvulsant that is used as adjunctive therapy in management of epilepsy and for neuropathic pain syndromes. Therapy with gabapentin is not associated with serum aminotransferase elevations, but several cases of clinically apparent liver injury from gabapentin have been reported. Antiepileptics such as gabapentin and pregabalin are sometimes used to treat neuropathic pain. The LiverTox, an authoritative resource for drug-induced liver injury, classifies these 2 agents as class C, indicating that clinically apparent liver injury is uncommon. 55, 56 Mechanistically, both agents are likely safe to use in hepatic impairment, as they are primarily renally eliminated in an Gabapentin/pregabalin: not metabolized by the liver or bound by proteins, but consider renal dysfunction in cirrhosis patients, as well as other relevant side effects (e.g. sedation, dizziness); minimal data on safety of these agents. Pain management in patients with cirrhosis is a difficult clinical challenge for health care professionals, and few prospective studies have offered an evidence-based approach. In patients with end-stage liver disease, adverse events from analgesics are frequent, potentially fatal, and often avoidable. Severe complications from analgesia in these patients include hepatic encephalopathy Carbamazepine has been reported to cause hepatotoxicity in the general population; it may precipitate a rapid deterioration in cirrhotic patients and thus should be avoided. 46 Gabapentin is unique among many anticonvulsants because it is not metabolized by the liver or bound to plasma proteins, making it a preferred anticonvulsant in patients Pain is prevalent in patients with cirrhosis. Due to potential alterations in drug metabolism, risk for adverse effects, and complications from cirrhosis, physicians are often faced with difficult choices when choosing appropriate analgesics in these patients. Overall, acetaminophen remains the preferred analgesic. Despite its potential for intrinsic liver toxicity, acetaminophen is safe when for short duration. Gabapentin and pregabalin are generally safe. Duloxetine should be avoided in hepatic impairment. Topical diclofenac and lidocaine seem to be safe in patients with cirrhosis. 2023 Published by Elsevier Inc. The American Journal of Medicine (2024) 137:99−106 KEYWORDS: Analgesic; Cirrhosis; Drug safety; Pain management The therapeutic use of analgesics in patients with liver cirrhosis: a literature review and evidence-based recommendations. Hepatitis monthly. 2014 Oct;14(10) doi: 10.5812/hepatmon.23539. Recent review of pain management in cirrhosis. Gabapentin is an uncommon cause of DILI reported to cause a hepatocellular, cholestatic, or mixed picture of liver injury. Given the limitations of prior cases, we feel our report most closely ties gabapentin use to the resultant transaminase elevation. Someone with cirrhosis, a severe form of liver damage, must be very careful when taking prescription or over-the-counter (OTC) medications. This article looks at the various medications for Gabapentin isn’t known to harm the liver. While there have been some individual reports of liver damage from gabapentin, it’s considered extremely rare. However, one possible side effect of gabapentin may cause liver damage. This side effect is a reaction called DRESS (drug reaction with eosinophilia and systemic symptoms) syndrome. It’s INTRODUCTION. Chronic pain in cirrhosis is common, poorly characterized, and uniquely morbid. Reported by 40%–79% of patients with cirrhosis, 1,2 it is a key driver of poor functional status and quality of life. 3–6 Patients with cirrhosis and chronic pain also have significantly greater health care use. 7 Pain management in cirrhosis can be complex because of challenges in diagnosis and Gabapentin and pregabalin are safe; use cautiously in patients with hepatic encephalopathy. Topical lidocaine and diclofenac are safe. Pain is common and affects 30%-79% 1 of patients with cirrhosis. Gabapentin or pregabalin may be better tolerated in cirrhosis because of non-hepatic metabolism and a lack of anti-cholinergic side effects. Keywords: analgesia; drug-induced liver injury; liver cirrhosis; paracetamol. What does gabapentin have to do with any of that? The itching is from the cirrhosis What you need for that is an antihistamine. Carbamazepine is associated with hepatotoxicity and should be avoided in patients with liver dysfunction. Gabapentin is the preferred agent, as it is not metabolized hepatically nor protein bound, but should be adjusted according to renal function. 4. Summary and Recommendations Drug metabolism in cirrhosis. The liver plays a major role in the distribution and elimination of most drugs (Table 1) and the more advanced the liver disease, the greater the impairment in drug metabolism. 3 This occurs because of a reduction in hepatic blood flow, porto-systemic shunting, and a reduction in number and function of existing We would like to show you a description here but the site won’t allow us. While there are no cures for the late-stage liver disease there are various treatment options including gabapentin and cirrhosis of the liver. One of the main goals of cirrhosis treatment is to ease the symptoms. Some options include avoiding alcohol, a low-salt diet, and weight loss. This class, which includes gabapentin and pregabalin, is not metabolized by the liver. Therefore, risks in patients with advanced liver disease are not greatly increased. However, there are case reports of pregabalin‐induced hepatoxicity. 4 Gabapentin and pregabalin are renally excreted, so dosages need to be adjusted for renal failure.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |