Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
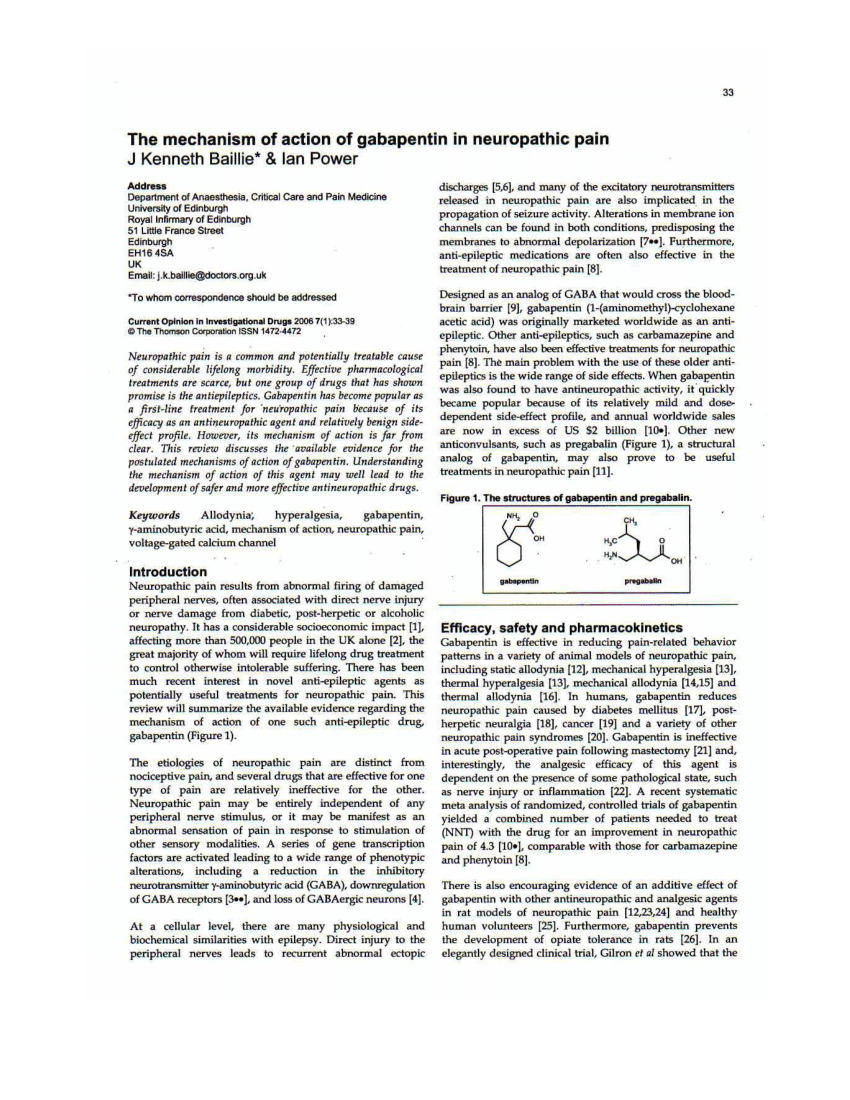
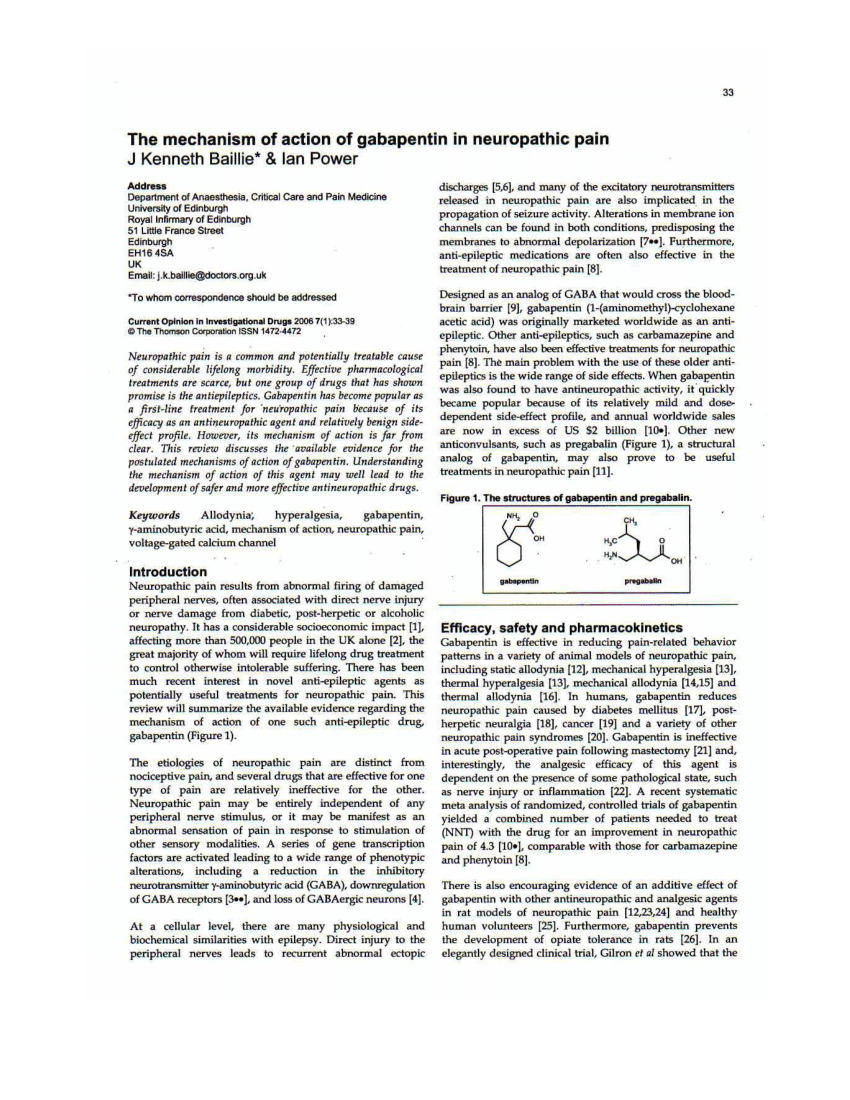
Herein we review the current understanding of the state‐dependent mechanisms of the gabapentinoids, the pathophysiological role of their molecular target, the α 2 δ calcium channel subunit, and the implications for clinical usage. Instead, it exhibits several distinct pharmacological activities, including: (1) binding to the alpha-2-delta protein subunit of voltage-gated calcium channels in the central nervous system, thereby blocking the excitatory influx of calcium; (2) reducing the expression and phosphorylation of CaMKII via modulation of ERK1/2 phosphorylation; (3 Originally designed as analogs of GABA, the gabapentinoids bind to the α 2 δ-1 and α 2 δ-2 auxiliary subunits of calcium channels, though only the former has been implicated in the development of neuropathy in animal models. The binding to α2δ-1 subunits inhibits nerve injury-induced trafficking of α1 pore forming units of calcium channels (particularly N-type) from cytoplasm to plasma membrane (membrane trafficking) of pre-synaptic terminals of dorsal root ganglion (DRG) neurons and dorsal horn neurons. GBP and PGB exert their analgesic actions by selectively binding the α 2 δ 1 auxiliary subunit of voltage-sensitive calcium channels, thereby inhibiting channel function. Numerous tissues express the α 2 δ 1 subunit where GBP and PGB can alter calcium-mediated signaling events. Mechanism of action. Gabapentin has no direct GABAergic action and does not block GABA uptake or metabolism. Gabapentin blocks the tonic phase of nociception induced by formalin and carrageenan, and exerts a potent inhibitory effect in neuropathic pain models of mechanical hyperalgesia and mechanical/thermal allodynia. The binding to α2δ-1 subunits inhibits nerve injury-induced trafficking of α1 pore forming units of calcium channels (particularly N-type) from cytoplasm to plasma membrane (membrane trafficking) of pre-synaptic terminals of dorsal root ganglion (DRG) neurons and dorsal horn neurons. Mechanism of action. Gabapentin has no direct GABAergic action and does not block GABA uptake or metabolism. Gabapentin blocks the tonic phase of nociception induced by formalin and carrageenan, and exerts a potent inhibitory effect in neuropathic pain models of mechanical hyperalgesia and mechanical/thermal allodynia. Gabapentin binds to a 2d receptors with greater affinity to the a 2d-1 subtype.22 Mutations of a 2d-1 or a 2d-2 block the neuronal actions of gabapentin by prevent-ing its binding, but not mutations in a 2d-3, indicating that the effects are mediated by a 2d subunits of VGCCs.23 Several other sites of action have been described, such as NMDA Mechanism of action. The precise mechanism through which gabapentin exerts its therapeutic effects is unclear. 16,17 The primary mode of action appears to be at the auxillary α2δ-1 subunit of voltage-gated calcium channels (though a low affinity for the α2δ-2 subunit has also been reported). 10,8,14 The major function of these subunits is Mechanistically, the effect of gabapentin is to blunt the Ca v α 2 δ-1 mediated regulation of forward and reverse trafficking of the N-type calcium channel Ca v 2.2 subunit — a calcium channel Gabapentin is an anti-epileptic drug but its use has expanded to treat multiple other diseases including post-herpetic neuralgia, neuropathic pain, and spasticity. The mechanism of action is not fully understood but may be related to gabapentin’s action on calcium channels leading to diminution of excitatory neurotransmitters. The interaction of gabapentin and pregabalin with conventional antiepileptic and analgesic drug targets is likely to be modest, at best, and has been largely dismissed in favour of a selective inhibitory effect on voltage-gated calcium channels containing the α 2 δ-1 subunit. This mechanism is consistently observed in both rodent- and human Gabapentinoids are being increasingly used as adjuncts for management of perioperative pain. Although gabapentinoids are classed as calcium channel blockers, their mechanisms of action are poorly understood. The analgesic effect in neuropathic pain is well evidenced but the role in postoperative pain is less certain. Gabapentinoids are being increasingly used as adjuncts for management of perioperative pain. Although gabapentinoids are classed as calcium channel blockers, their mechanisms of action are poorly understood. The analgesic effect in neuropathic pain is well evidenced but the role in postoperative pain is less certain. Preferential action of gabapentin and pregabalin at P/Q-type voltage-sensitive calcium channels: inhibition of K +-evoked [3 H]-norepinephrine release from rat neocortical slices. Synapse 45, 171–190. 10.1002/syn.10094 [ DOI ] [ PubMed ] [ Google Scholar ] Mechanisms of action. Gabapentin and pregabalin do not bind to GABA receptors despite their structural similarity but have a high affinity for the α2δ-1 subunit of voltage-gated calcium channels (VGCCs). 19 VGCCs are composed of multiple subunits: α 1, β, γ and α 2 δ. Voltage-hated calcium channels, which therefore decreases the release of excitatory neurotransmitters. Mechanism of action: By inhibiting the voltage-gated calcium channels in the CNS, gabapentin reduces the release of excitatory neurotransmitters (mostly noradrenaline, dopamine and serotonin), and therefore decreases epileptogenesis. Clinical Mechanism of Action. Although the exact mechanism of action with the GABA receptors is unknown, researchers know that gabapentin freely passes the blood-brain barrier and acts on neurotransmitters. Gabapentin has a cyclohexyl group to the structure of the neurotransmitter GABA as a chemical structure. Gabapentin is an antiepileptic drug (AED) by design expected to mimic the action of the neurotransmitter gamma-aminobutyric acid (GABA). However, its principal proposed mechanism of action is the interaction with the alpha 2-delta subunit of L-type voltage-regulated calcium channels.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |