Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 | 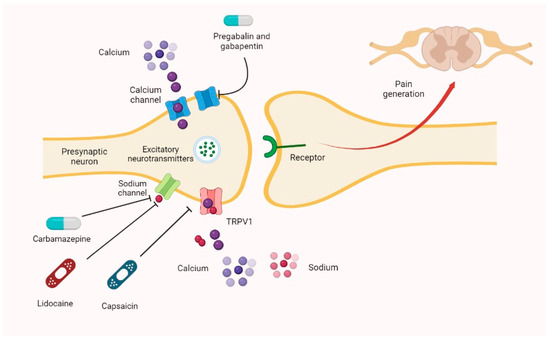 |
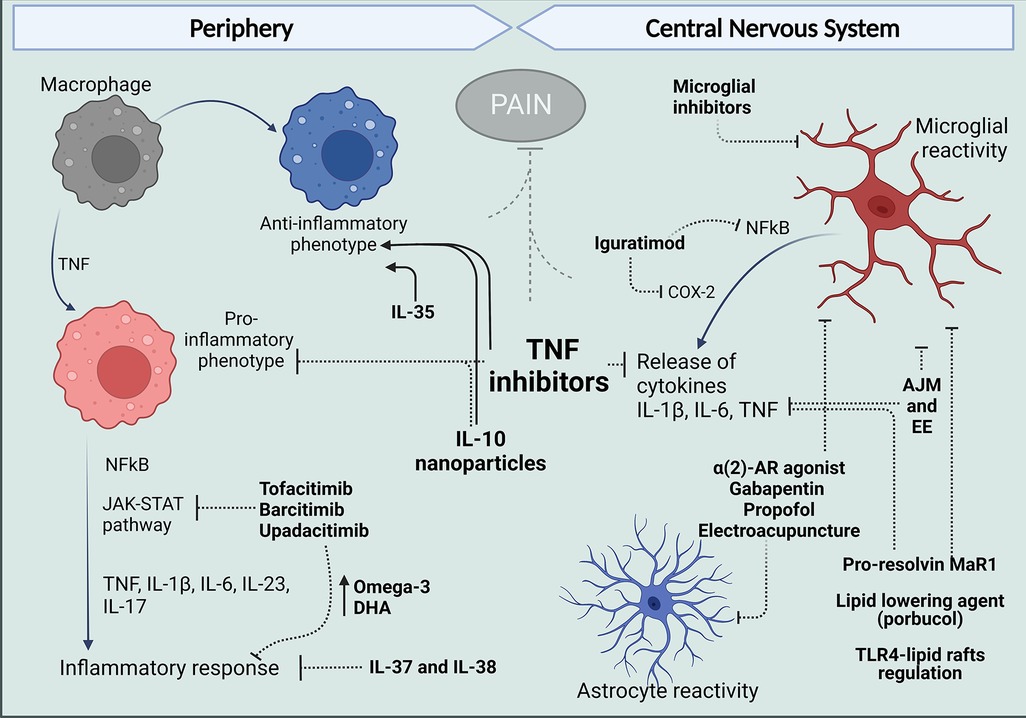
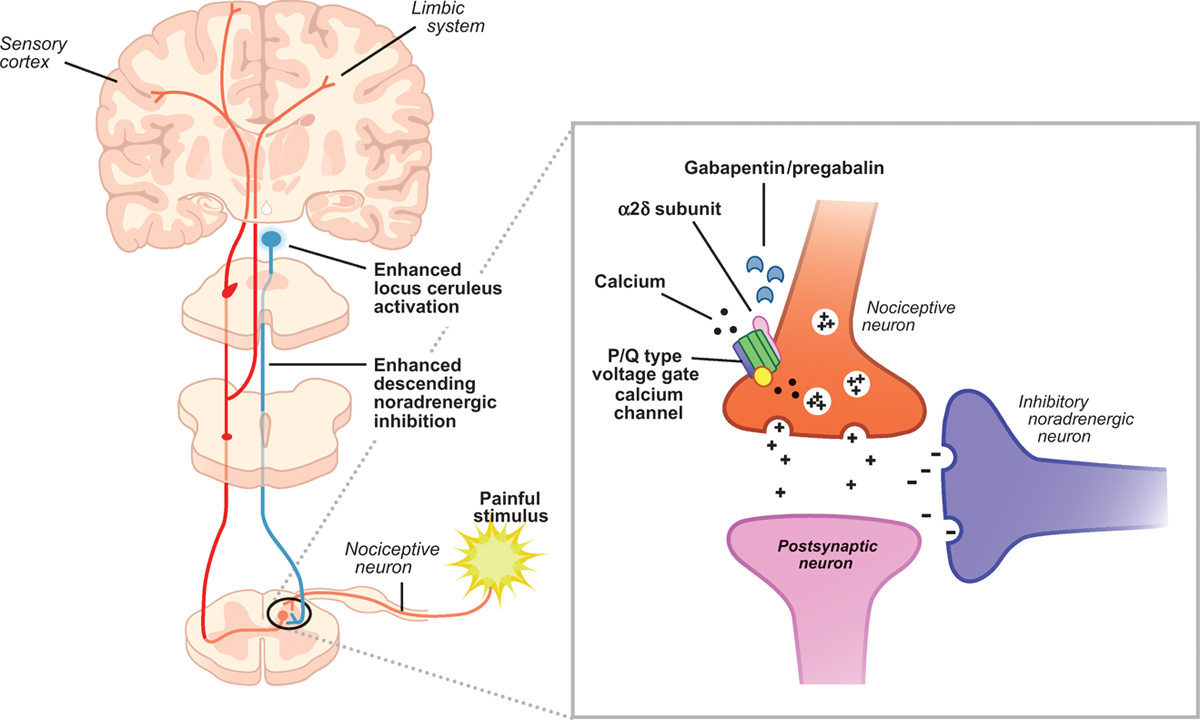
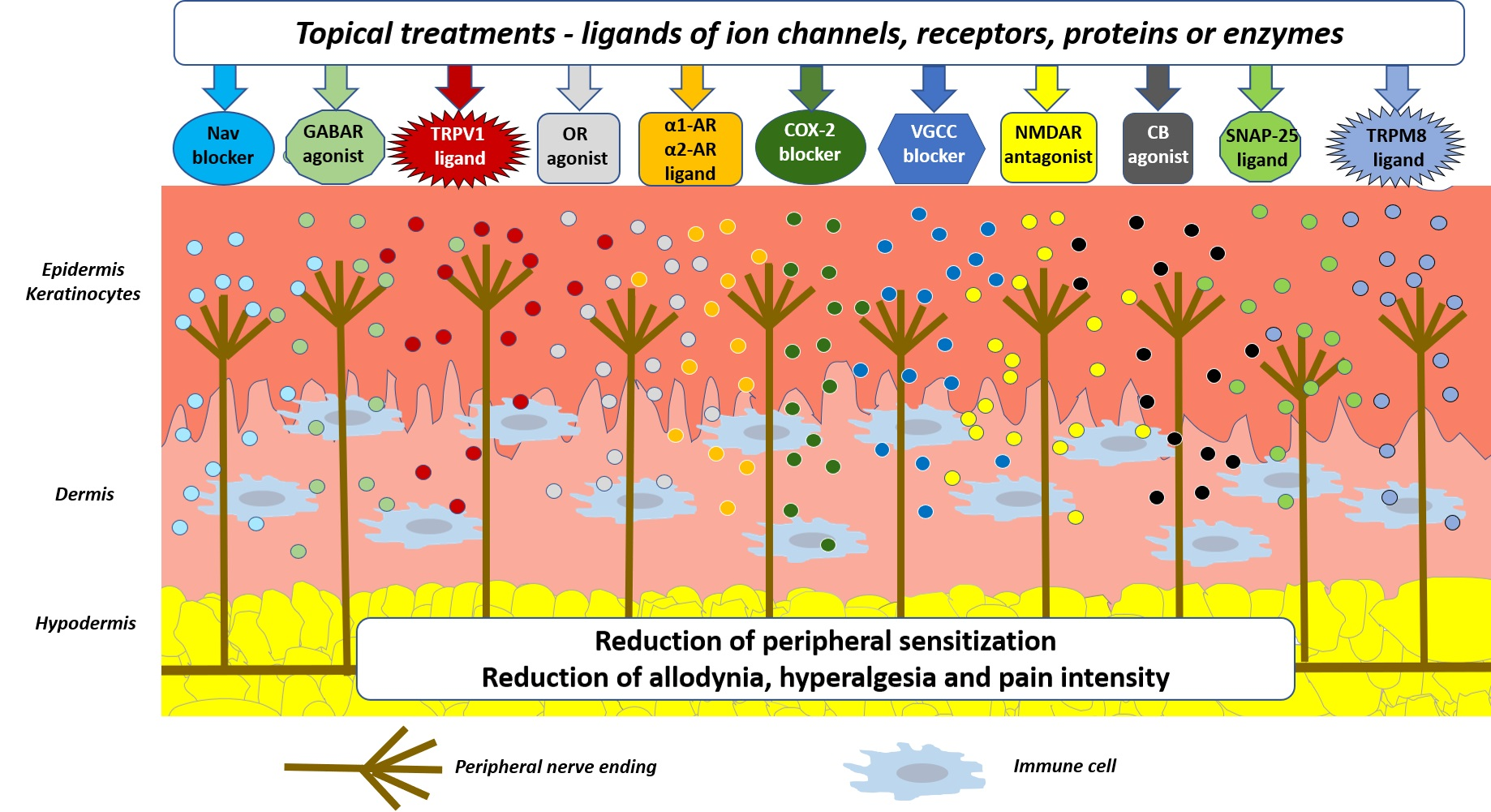
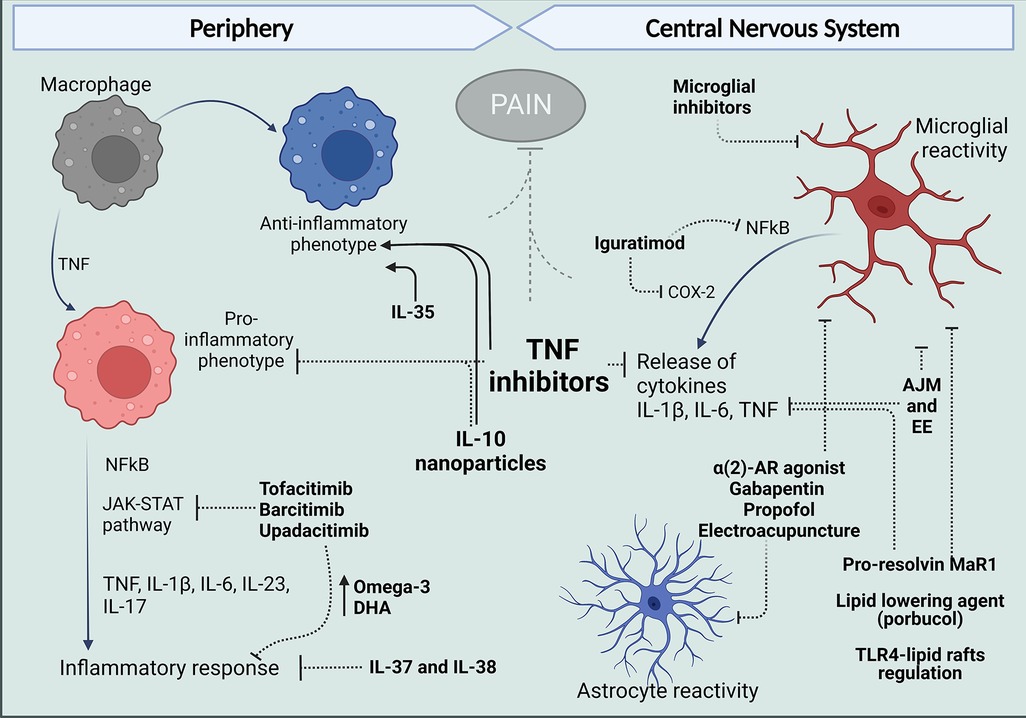
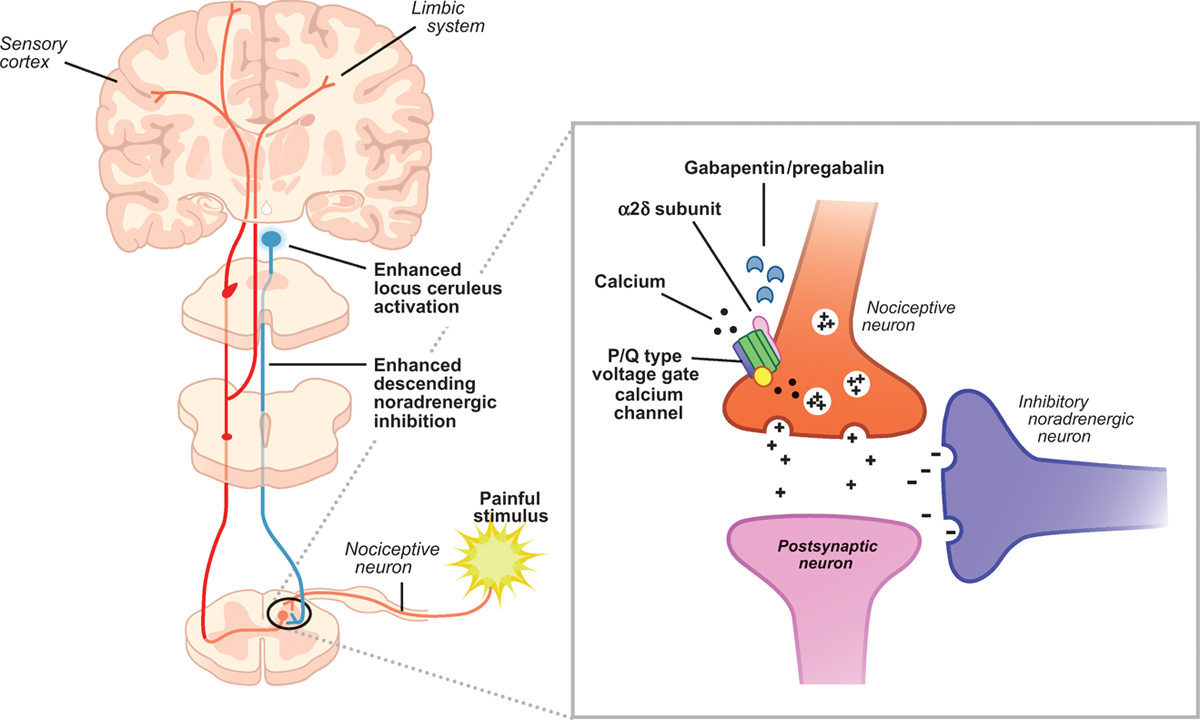
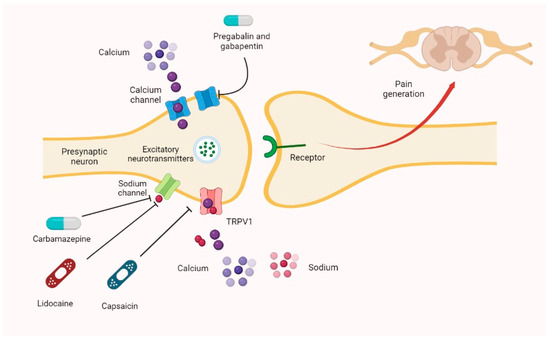
Postherpetic neuralgia: Management of postherpetic neuralgia (PHN) in adults. Seizures, focal (partial) onset (immediate release only): As adjunctive therapy in the treatment of focal (partial) seizures with and without secondary generalization in adults and pediatric patients 3 years of age and older with epilepsy. The analgesic effect in neuropathic pain is well evidenced but the role in postoperative pain is less certain. Medline and EMBASE database searches were conducted to identify studies relating to mechanisms of action and effects in experimental animal models of inflammatory and postoperative pain and human models of experimental pain. Mechanism of action. The precise mechanism through which gabapentin exerts its therapeutic effects is unclear. 16,17 The primary mode of action appears to be at the auxillary α2δ-1 subunit of voltage-gated calcium channels (though a low affinity for the α2δ-2 subunit has also been reported). 10,8,14 The major function of these subunits is Mechanism of action. Gabapentin has no direct GABAergic action and does not block GABA uptake or metabolism. Gabapentin blocks the tonic phase of nociception induced by formalin and carrageenan, and exerts a potent inhibitory effect in neuropathic pain models of mechanical hyperalgesia and mechanical/thermal allodynia. Gabapentin is commonly used to treat neuropathic pain (pain due to nerve damage). This review updates a review published in 2014, and previous reviews published in 2011, 2005 and 2000. To assess the analgesic efficacy and adverse effects of Understanding how gabapentin works for pain is crucial for those exploring treatment options for conditions like neuropathic pain, fibromyalgia, and even post-surgical discomfort. The Mechanism of Action. Gabapentin's primary mechanism revolves around its interaction with calcium channels in the nervous system. In randomized open clinical trial, the combination of gabapentin with opioid analgesics was shown to provide better relief in neuropathic pain in cancer patients as compared to opioid analgesics alone in terms of reduction in pain intensity for burning and shooting pain at different days of the study. I appreciate the comments of Gazulla et al. regarding my focused review on the mechanisms of action and side effects of gabapentinoids. 1 I cited the article by Yu et al., as they found that gabapentin increases expression of delta subunit-containing GABAA receptors. 2 I am also aware of the placebo-controlled pilot study of Gazulla et al. regarding the potential benefit of pregabalin for Mechanism of Action. Gabapentin's exact mechanism of action is not fully understood, but it is believed to work by reducing abnormal electrical activity in the brain. It is thought to bind to calcium channels, modulating their activity and reducing the release of neurotransmitters involved in seizures and nerve pain. Gabapentin is an anti-epileptic agent but now it is also recommended as first line agent in neuropathic pain, particularly in diabetic neuropathy and post herpetic neuralgia. α2δ-1, an auxillary subunit of voltage gated calcium channels, has been documented as its main target and its specific binding to this subunit is described to produce Gabapentin prevents pain responses in several animal models of hyperalgesia and prevents neuronal death in vitro and in vivo with models of the neurodegenerative disease amyotrophic lateral sclerosis (ALS). Gabapentin is also active in models that detect anxiolytic activity. This activity outlines the indications, mechanisms of action, administration, significant adverse effects, contraindications, monitoring, and characteristics of gabapentin toxicity. The analgesic effect in neuropathic pain is well evidenced but the role in postoperative pain is less certain. Medline and EMBASE database searches were conducted to identify studies relating to mechanisms of action and effects in experimental animal models of inflammatory and postoperative pain and human models of experimental pain. Gabapentin has become popular as a first-line treatment for neuropathic pain because of its efficacy as an antineuropathic agent and relatively benign side-effect profile. However, its mechanism of action is far from clear. This review discusses the available evidence for the postulated mechanisms of action of gabapentin. Mechanisms of action. Gabapentin and pregabalin do not bind to GABA receptors despite their structural similarity but have a high affinity for the α2δ-1 subunit of voltage-gated calcium channels (VGCCs). 19 VGCCs are composed of multiple subunits: α 1, β, γ and α 2 δ. The focus of perioperative pain management should be to attempt to minimise the nociceptive input and reduce the risk of transition to central sensitisation. Gabapentinoids are being increasingly used as adjuncts for management of perioperative pain. Although gabapentinoids are classed as calcium channel blockers, their mechanisms of action are poorly understood. The analgesic effect in Mechanism of action. Gabapentin has no direct GABAergic action and does not block GABA uptake or metabolism. Gabapentin blocks the tonic phase of nociception induced by formalin and carrageenan, and exerts a potent inhibitory effect in neuropathic pain models of mechanical hyperalgesia and mechanical/thermal allodynia. Targeted Use of Gabapentin. One of the most commonly cited uses of gabapentin in veterinary medicine is for treating acute post-operative pain. 5 Considering the mechanism of action of gabapentin and its impact on pain signaling, it is unlikely that gabapentin will be an effective analgesic in this context. Inflammation is the most common Gabapentinoids depress neuronal excitability through interactions with the a2d-1 calcium channel subunit, stimulate descending inhibition, inhibit descending serotonergic facilitation, inhibit inflammatory media-tors, and influence the affective component of pain. Multiple dose gabapentin attenuates cutaneous pain and central sensitisation but not muscle pain in healthy volunteers. Pain 125: 158–164. [ DOI ] [ PubMed ] [ Google Scholar ]
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |