Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
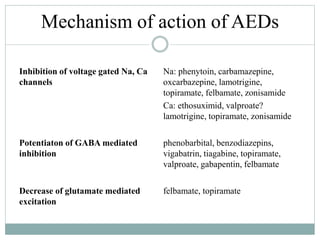 | 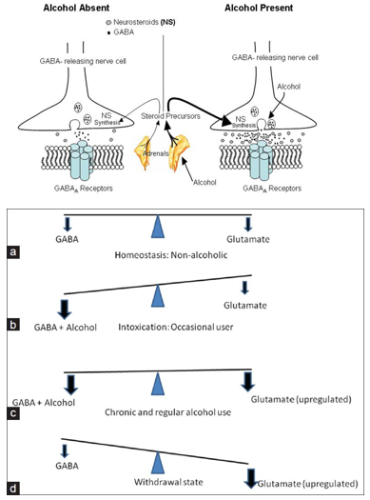 |
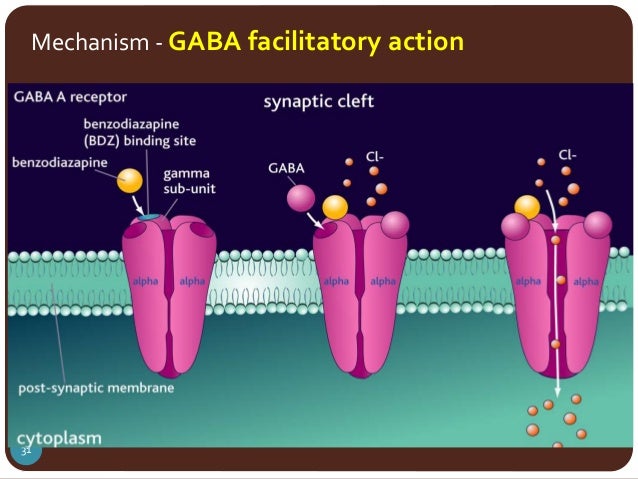
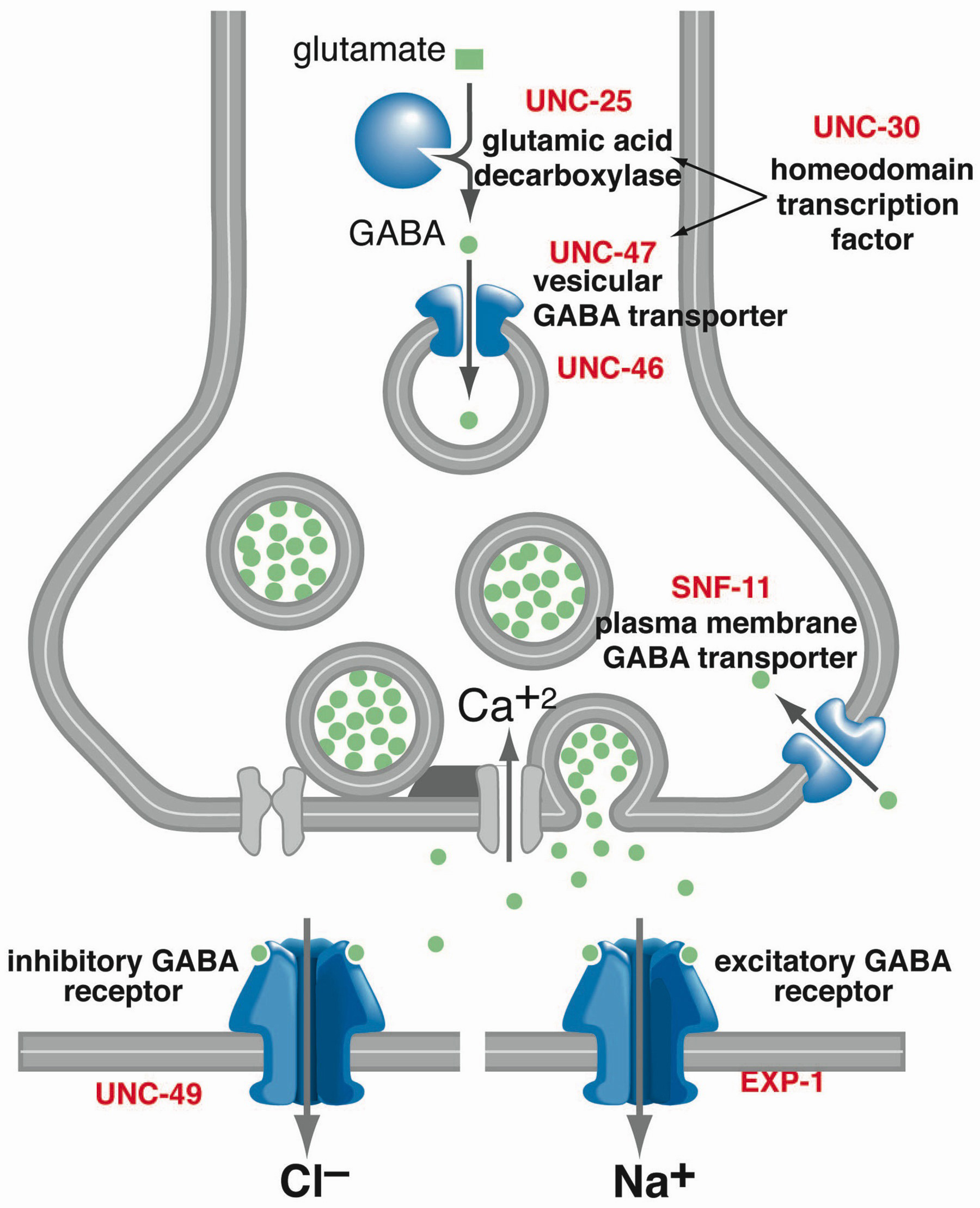
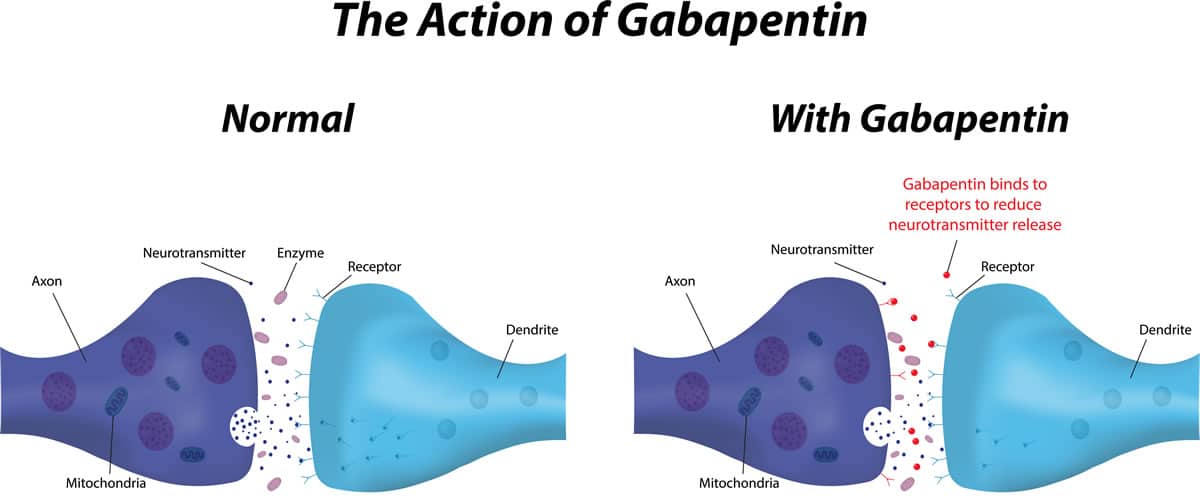
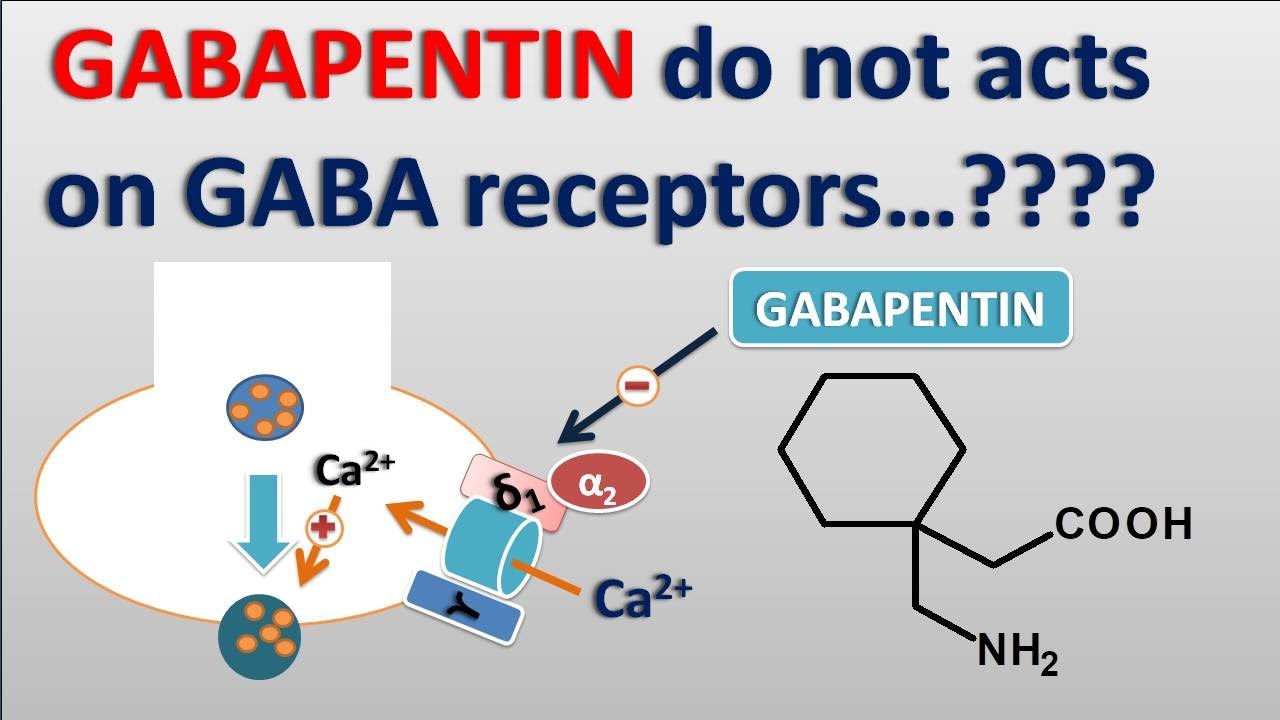
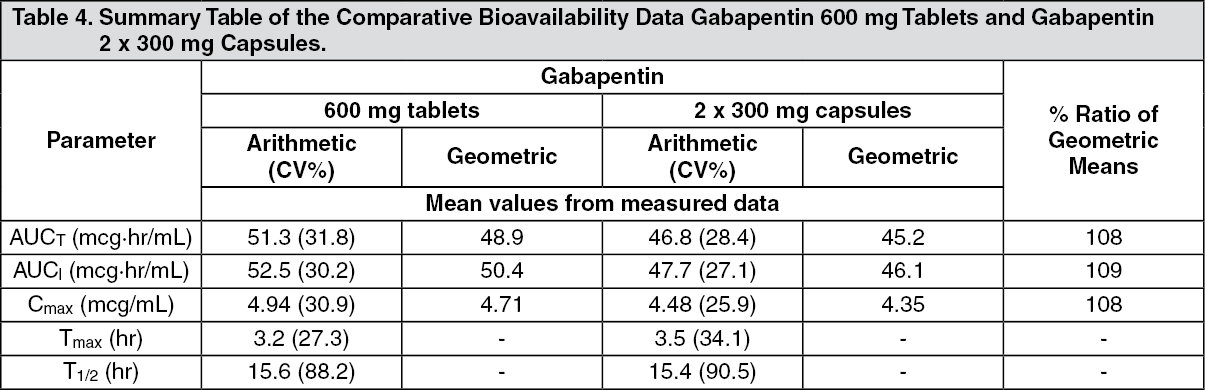
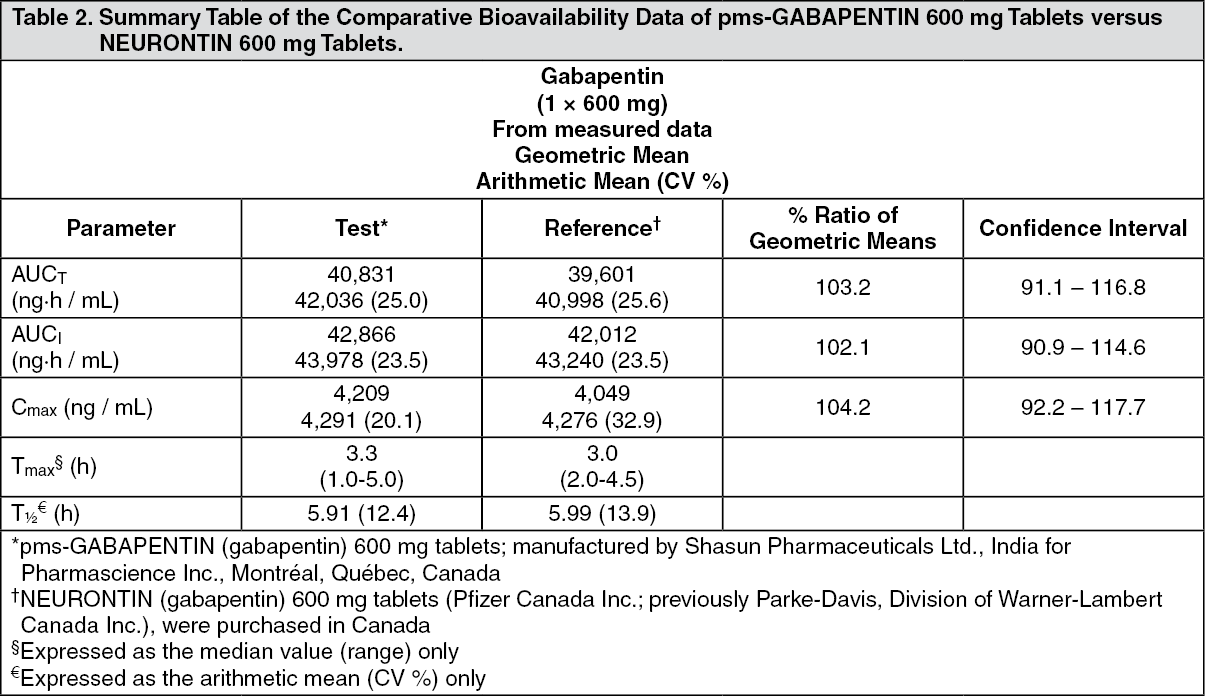
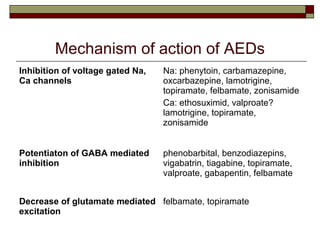
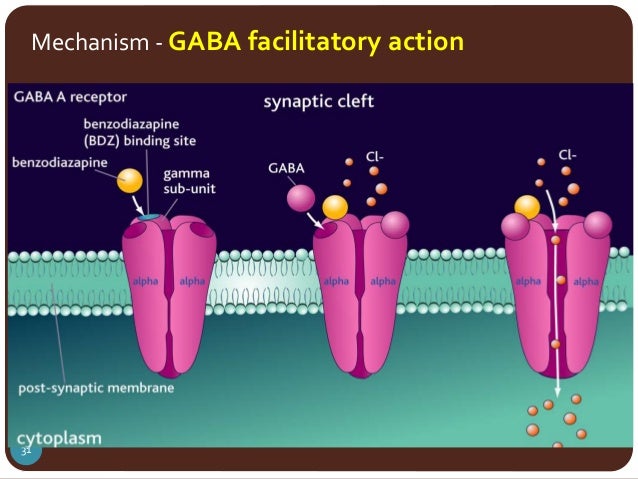
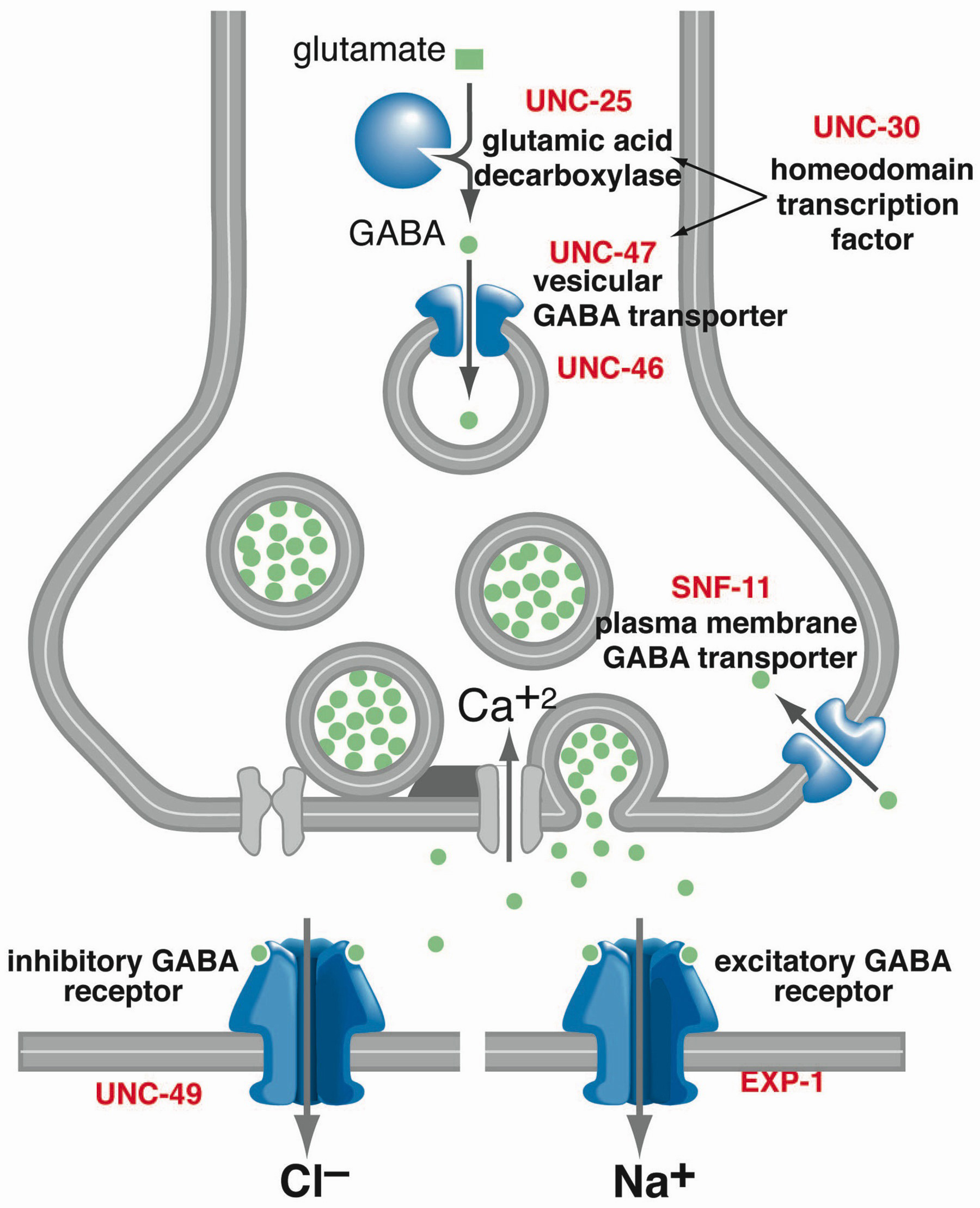
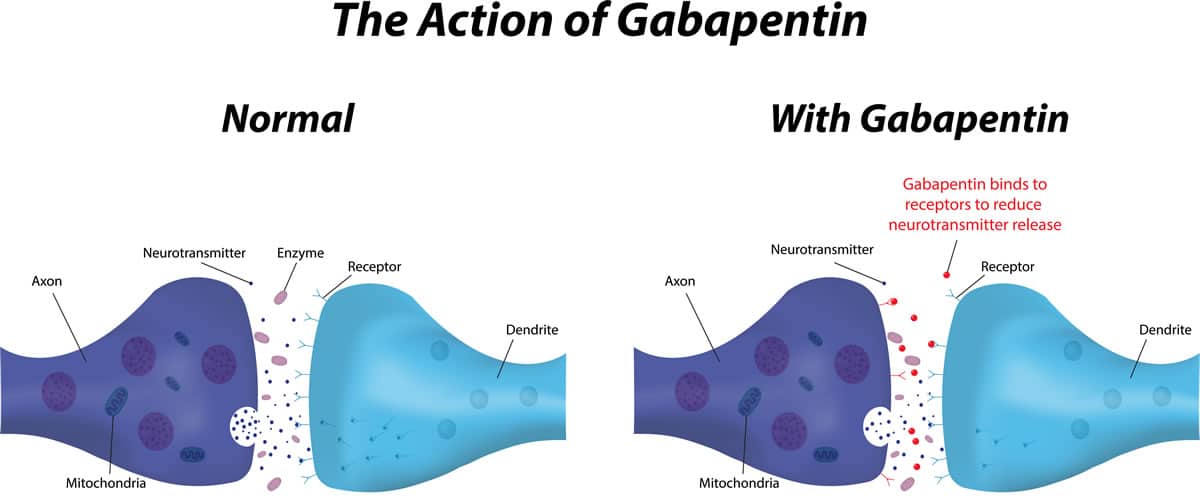
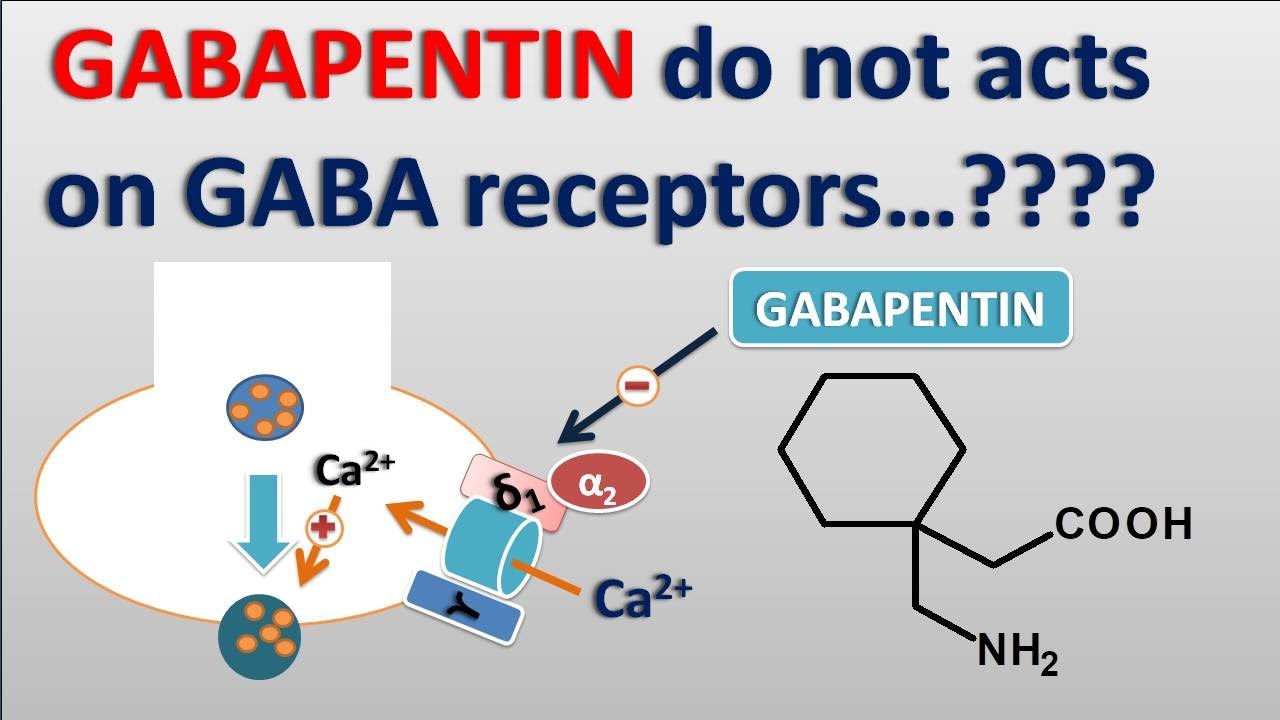
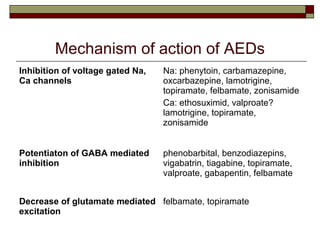
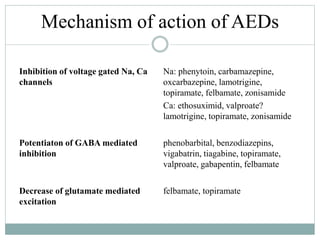
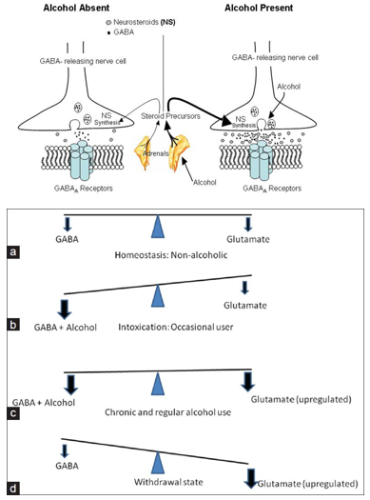
Mechanism of action. The precise mechanism through which gabapentin exerts its therapeutic effects is unclear. 16,17 The primary mode of action appears to be at the auxillary α2δ-1 subunit of voltage-gated calcium channels (though a low affinity for the α2δ-2 subunit has also been reported). 10,8,14 The major function of these subunits is Mechanism of Action Although gabapentin is a structural analog of the neurotransmitter gamma-aminobutyric acid (GABA), it appears not to interact with GABA receptors. Its mechanism of action is not entirely clear but is likely related to inhibition of calcium and, possibly, sodium channels. 1 Although the cellular mechanisms of pharmacological actions of gabapentin (Neurontin ®) remain incompletely described, several hypotheses have been proposed. It is possible that different mechanisms account for anticonvulsant, antinociceptive, anxiolytic and neuroprotective activity in animal models. Mechanism of action: By inhibiting the voltage-gated calcium channels in the CNS, gabapentin reduces the release of excitatory neurotransmitters (mostly noradrenaline, dopamine and serotonin), and therefore decreases epileptogenesis. Clinical effects Mechanism of Action. Gabapentin is structurally related to GABA. However, it does not bind to GABA A or GABA B receptors, and it does not appear to influence synthesis or uptake of GABA. High affinity gabapentin binding sites have been located throughout the brain; these sites correspond to the presence of voltage-gated calcium channels Gabapentin is an anti-epileptic drug but its use has expanded to treat multiple other diseases including post-herpetic neuralgia, neuropathic pain, and spasticity. The mechanism of action is not fully understood but may be related to gabapentin’s action on calcium channels leading to diminution of excitatory neurotransmitters. Mechanism of action. Gabapentin has no direct GABAergic action and does not block GABA uptake or metabolism. Gabapentin blocks the tonic phase of nociception induced by formalin and carrageenan, and exerts a potent inhibitory effect in neuropathic pain models of mechanical hyperalgesia and mechanical/thermal allodynia. Gabapentin and pregabalin are structurally related compounds with recognized efficacy in the treatment of both epilepsy and neuropathic pain. The pharmacological mechanisms by which these agents exert their clinical effects have, until recently, remained unclear. The interaction of gabapentin and pr Mechanism of action. Gabapentin has no direct GABAergic action and does not block GABA uptake or metabolism. Gabapentin blocks the tonic phase of nociception induced by formalin and carrageenan, and exerts a potent inhibitory effect in neuropathic pain models of mechanical hyperalgesia and mechanical/thermal allodynia. In vitro, gabapentin modulates the action of the GABA synthetic enzyme, glutamic acid decarboxylase (GAD) and the glutamate synthesizing enzyme, branched-chain amino acid transaminase. Results with human and rat brain NMR spectroscopy indicate that gabapentin increases GABA synthesis. Although the mechanism of gabapentin therapeutic action is unclear, human subjects studies suggest that its administration leads to an overall increase in central GABA levels. In neocortical tissue extracted from individuals with intractable epilepsy, gabapentin administration resulted in 13% increase in cellular GABA concentrations ( Errante Mechanism of Action. Gabapentin is designed as GABA analog (similar to pregabalin), which means it binds to the α2δ (alpha-2-delta) Gabapentin (GBP) was originally developed as a potential agonist for Gamma-Amino-Butyric-Acid (GABA) receptors, aiming to inhibit the activation of pain-signaling neurons. Contrary to initial expectations, it does not bind to GABA receptors. Instead, it exhibits several distinct pharmacological activities, including: (1) binding to the alpha-2-delta protein subunit of voltage-gated calcium Although the exact mechanism of action with the GABA receptors is unknown, researchers know that gabapentin freely passes the blood-brain barrier and acts on neurotransmitters. Gabapentin has a cyclohexyl group to the structure of the neurotransmitter GABA as a chemical structure. As with many other agents, GBP was licensed for the treatment of epilepsy with little or no understanding of its mechanism of action. Continued research and the parallel development of PGB have contributed to a contemporary pharmacological view of GBP (and PGB) as drugs with multiple modest cellular effects at therapeutic concentrations, but with a single predominant mechanism of action that Gabapentin is a potent activator of voltage-gated potassium channels KCNQ3 and KCNQ5, even at low nanomolar concentrations. However, this activation is unlikely to be the dominant mechanism of gabapentin's therapeutic effects. [90] Mechanisms of action. Gabapentin and pregabalin do not bind to GABA receptors despite their structural similarity but have a high affinity for the α2δ-1 subunit of voltage-gated calcium channels (VGCCs). 19 VGCCs are composed of multiple subunits: α 1, β, γ and α 2 δ. For topiramate, felbamate, retigabine, losigamone and stiripentol, GABA A R modulation is one of several possible antiseizure mechanisms. Allopregnanolone, a progesterone metabolite that enhances GABA A R function, led to the development of ganaxolone. Gabapentin is an anti-epileptic agent but now it is also recommended as first line agent in neuropathic pain, particularly in diabetic neuropathy and post herpetic neuralgia. α2δ-1, an auxillary subunit of voltage gated calcium channels, has been documented as its main target and its specific binding to this subunit is described to produce different actions responsible for pain attenuation Here we review the current understanding of the pathophysiological role of the α 2 δ‐1 subunit, the mechanisms of analgesic action of gabapentinoid drugs and implications for efficacy in the clinic. Despite widespread use, the number needed to treat for gabapentin and pregabalin averages from 3 to 8 across neuropathies.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |