Gallery
Photos from events, contest for the best costume, videos from master classes.
 | |
 |  |
 | |
 |  |
 |  |
 |  |
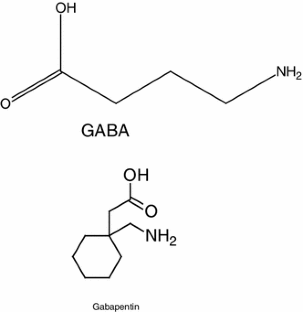
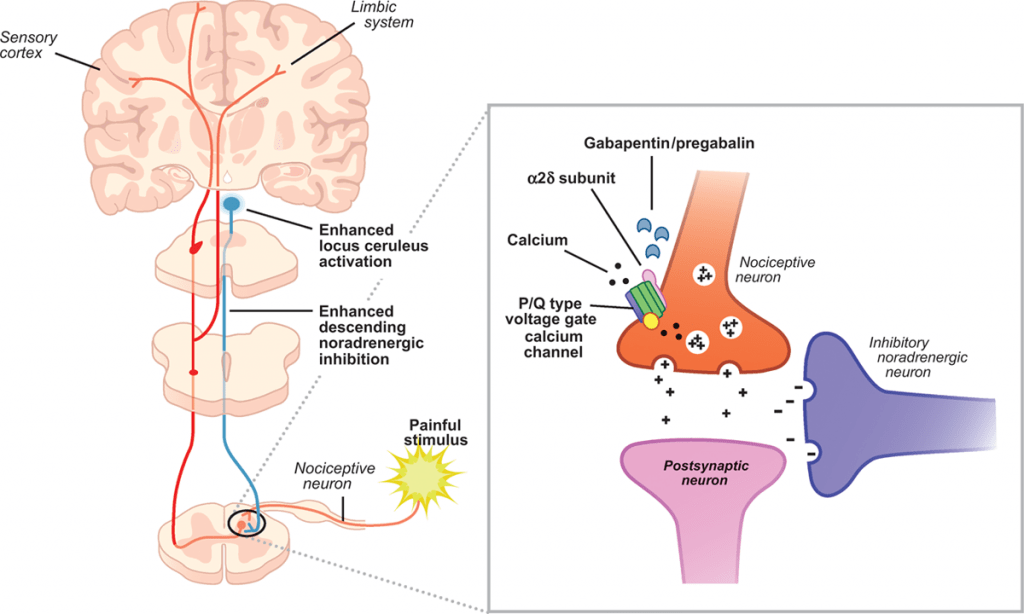
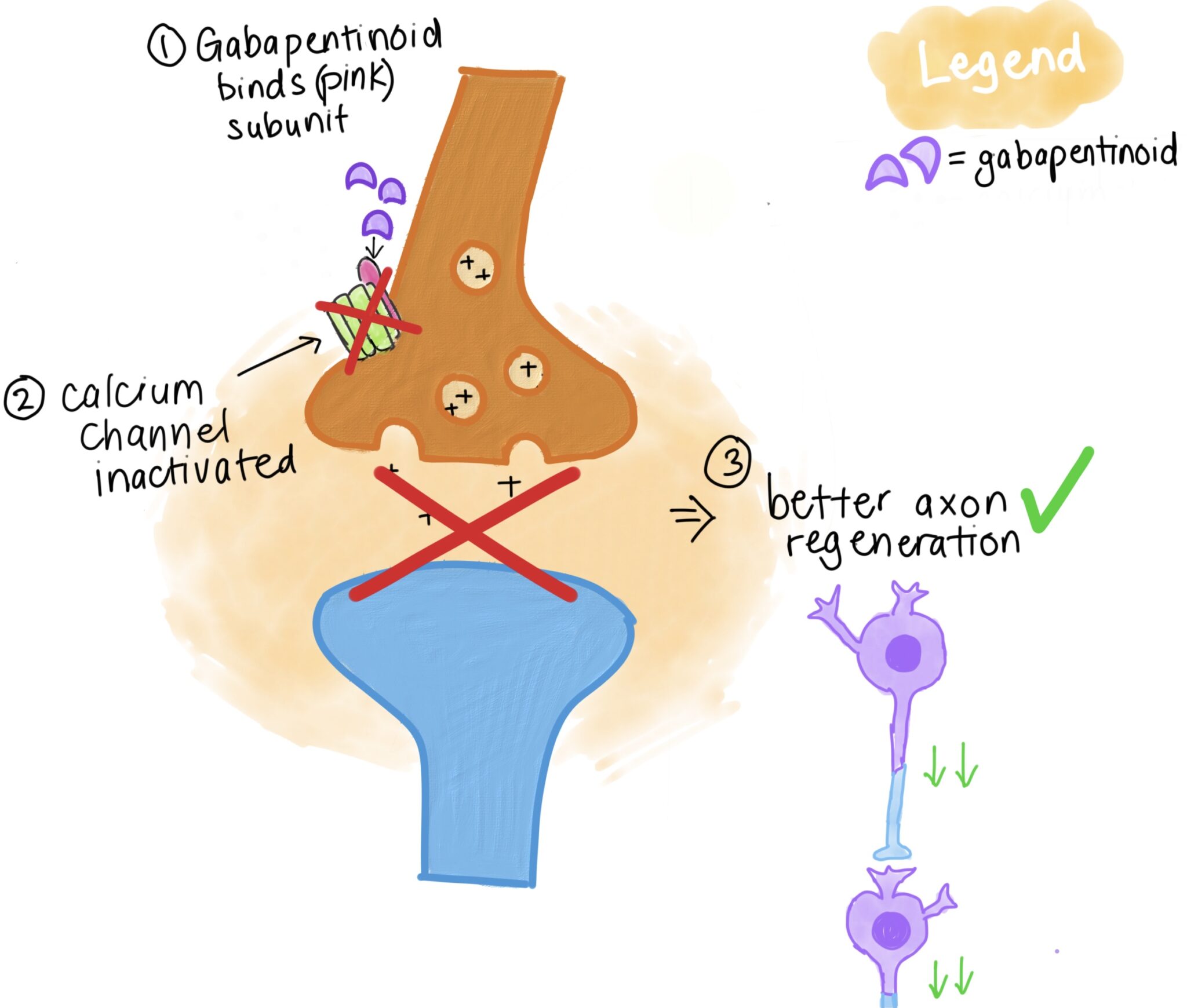
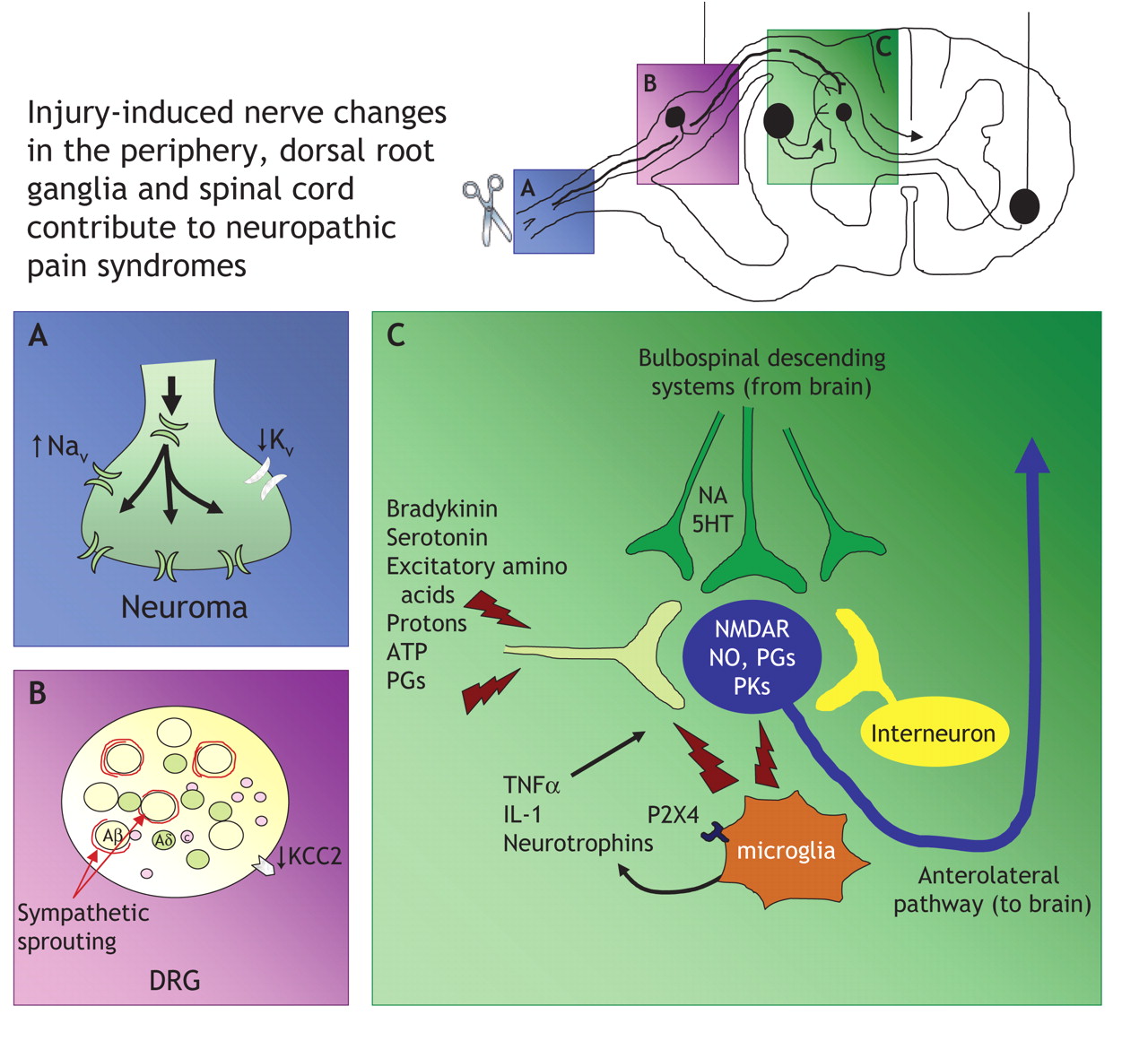
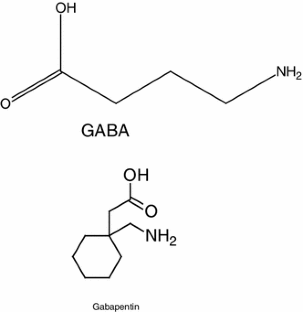
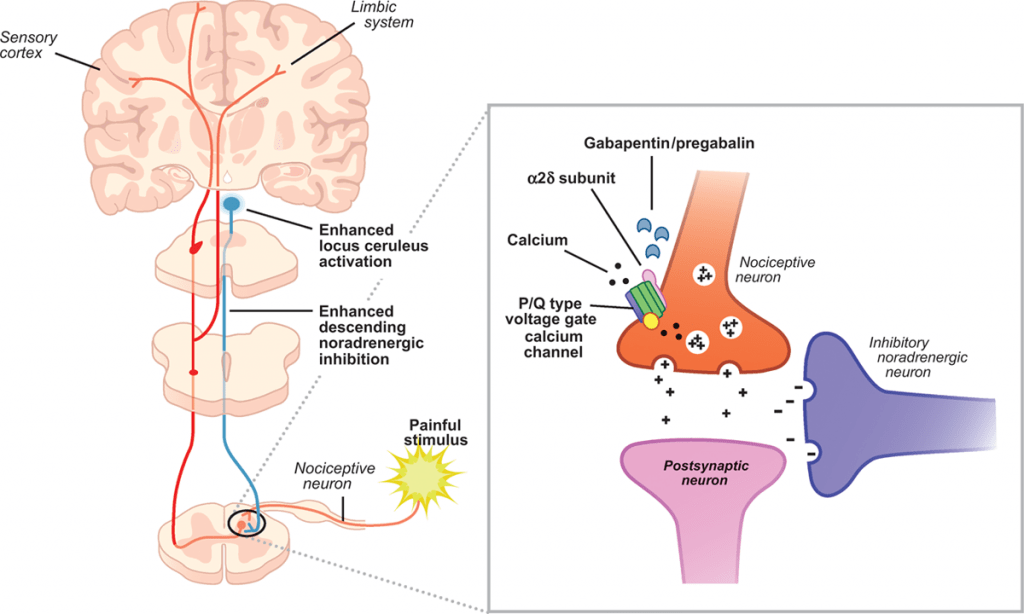
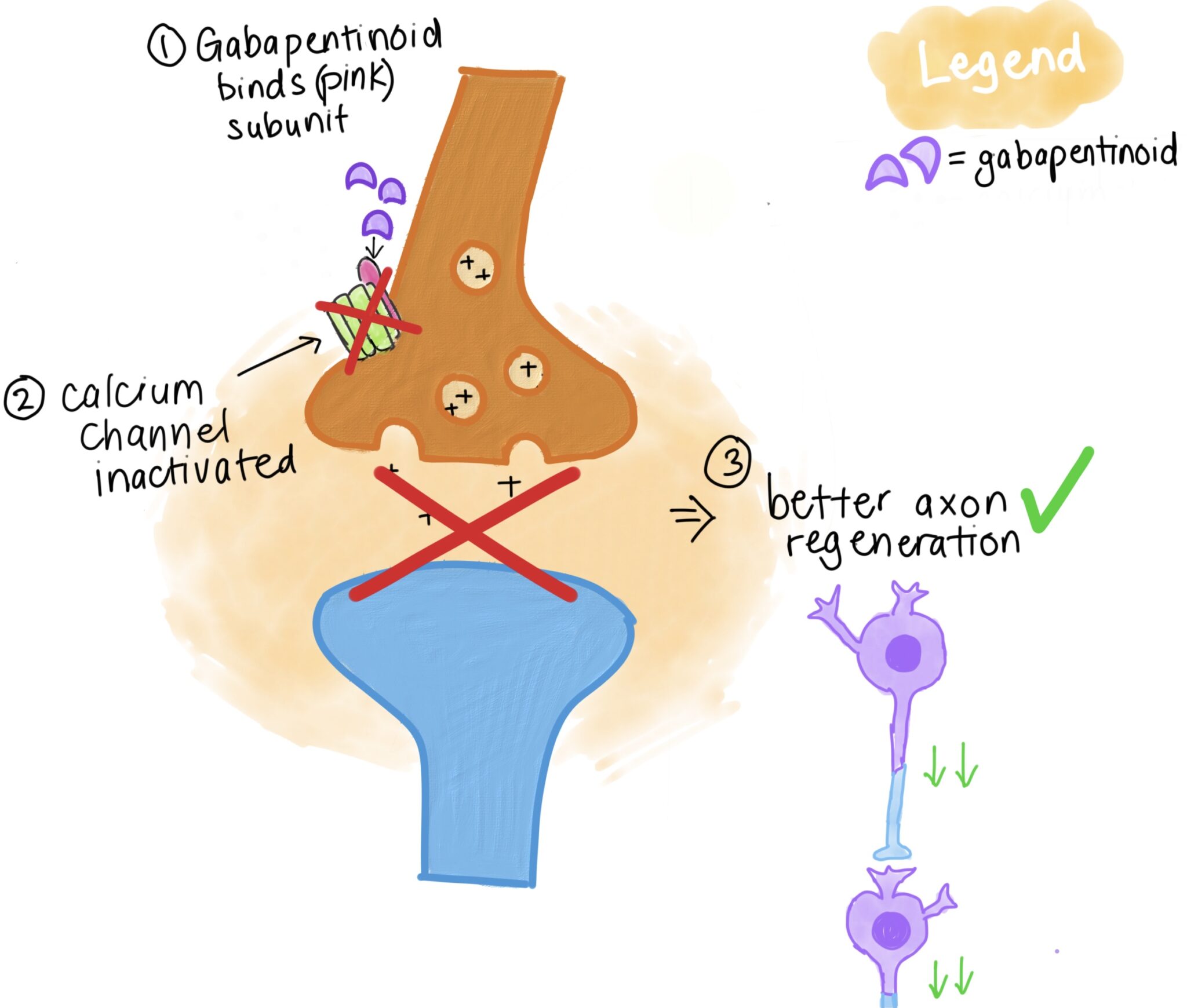
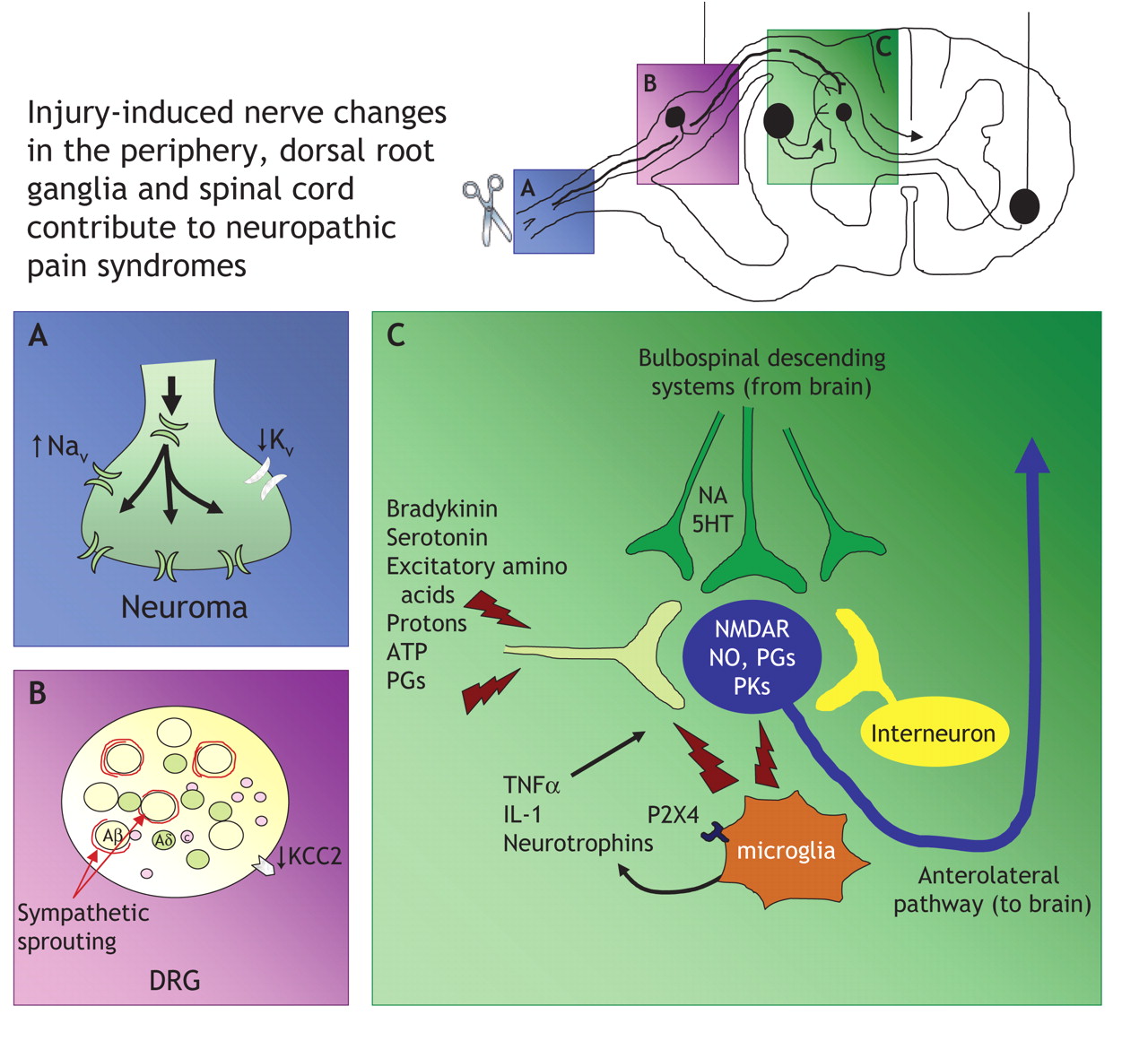
Gabapentin is an anticonvulsive medication that received approval from the US Food and Drug Administration (FDA) in 1993 and has been available in generic form in the USA since 2004. Gabapentin was originally used as a muscle relaxant and an anti-spasmodic. However, it was later discovered that gabapentin has the potential of an anticonvulsive medication and can be used as an adjunct to more Narrative: Neuropathic pain, when the pain generator is the nerve itself, occurs in a variety of conditions including diabetes mellitus and postherpetic neuropathy. The exact mechanism of action Mechanism of Action. Gabapentin's exact mechanism of action is not fully understood, but it is believed to work by reducing abnormal electrical activity in the brain. It is thought to bind to calcium channels, modulating their activity and reducing the release of neurotransmitters involved in seizures and nerve pain. The gabapentinoids are often recommended as first-line treatments for the management of neuropathic pain. The differing pharmacodynamic and pharmacokinetic profiles can have implications for clinical practice. This article has summarised these key Gabapentinoids are being increasingly used as adjuncts for management of peri-operative pain. Although gabapentinoids are classed as calcium channel blockers, their mechanisms of action are poorly understood. The analgesic effect in neuropathic pain is well evidenced but the role in postoperative pain is less certain. Gabapentin has been shown to be beneficial in treating several types of neuropathic pain; however, the mechanism of action by which gabapentin exerts its analgesic effect is still unknown.¹ It is suggested that gabapentin may block the calcium channel alpha(2)delta (a2d)-1 receptor in the brain. This protein-modulated receptor is involved in Gabapentin is an anti-epileptic agent but now it is also recommended as first line agent in neuropathic pain, particularly in diabetic neuropathy and post herpetic neuralgia. α2δ-1, an auxillary subunit of voltage gated calcium channels, has been documented as its main target and its specific binding to this subunit is described to produce Numerous studies confirm that gabapentinoids do not perturb normal detection and pain thresholds (Attal et al. 1998; Dirks et al. 2002); the pathophysiological state‐dependent effects of pregabalin and gabapentin implies other factors influence efficacy in neuropathic conditions. Gabapentin is commonly used to treat neuropathic pain (pain due to nerve damage). This review updates a review published in 2014, and previous reviews published in 2011, 2005 and 2000. To assess the analgesic efficacy and adverse effects of Neuropathic pain is a prevalent and burdensome condition, and both pregabalin and gabapentin are widely used for its treatment. However, there is a lack of clarity regarding their comparative efficacy and safety. This meta-analysis aims to evaluate and compare the effectiveness and safety of pregabalin vs. gabapentin in managing neuropathic pain. Gabapentin has become popular as a first-line treatment for neuropathic pain because of its efficacy as an antineuropathic agent and relatively benign side-effect profile. However, its mechanism of action is far from clear. Gabapentin is indicated for: Neuropathic pain caused by postherpetic neuralgia Adjunctive therapy in the treatment of partial seizures with or without secondary generalization; Neuropathic pain caused by diabetic peripheral neuropathy and spinal cord injury Restless leg syndrome (gabapentin enacarbil) Gabapentin is frequently used off-label for: The purpose of this report is to review the clinical evidence on the efficacy, safety and guidelines for use of gabapentin in adults with neuropathic pain, and to examine evidence on the misuse or abuse of gabapentin and other drugs for neuropathic pain. First-line drugs for neuropathic pain include antidepressants (tricyclic antidepressants and serotonin–noradrenaline reuptake inhibitors) and anticonvulsants acting at calcium channels (pregabalin and gabapentin). Gabapentin blocks the tonic phase of nociception induced by formalin and carrageenan, and exerts a potent inhibitory effect in neuropathic pain models of mechanical hyperalgesia and mechanical/thermal allodynia. Pharmacologic therapy for neuropathic pain, or nociplastic or centralized pain — For most patients with chronic neuropathic pain, initial treatment involves either selected antidepressants (ie, tricyclic antidepressants [TCAs] or serotonin-norepinephrine reuptake inhibitors [SNRIs]), or antiseizure medications (ie, gabapentin or pregabalin - Pain terms and definitions - Pharmacologic treatment based on type of pain - Mechanism-based analgesic targets - Recommended drug classes for treatment of neuropathic pain - Mechanisms of drugs for neuropathic pain - Comorbidities affecting drug choice for neuropathic pain - NSAIDs and acetaminophen: Usual oral dosing for adults Gabapentin (GBP) is a 3,3-disubstituted derivative of gamma-aminobutyric acid (GABA). It is recommended as a first-line treatment for chronic neuropathic pain, particularly in diabetic neuropathy Gabapentin is an anticonvulsant medication used in the management of peripheral neuropathic pains, postherpetic neuralgia, and partial-onset seizures. A recent study has shown the effectiveness of gabapentin (5 or 50 mg/kg, i.p.) in attenuating neuropathic pain behavior in forelimb neuropathic pain model (due to partial injury to medial and ulner nerves) in a dose-dependent manner (Yi et al. 2011).
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 | |
 |  |
 | |
 |  |
 |  |
 |  |