Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 | 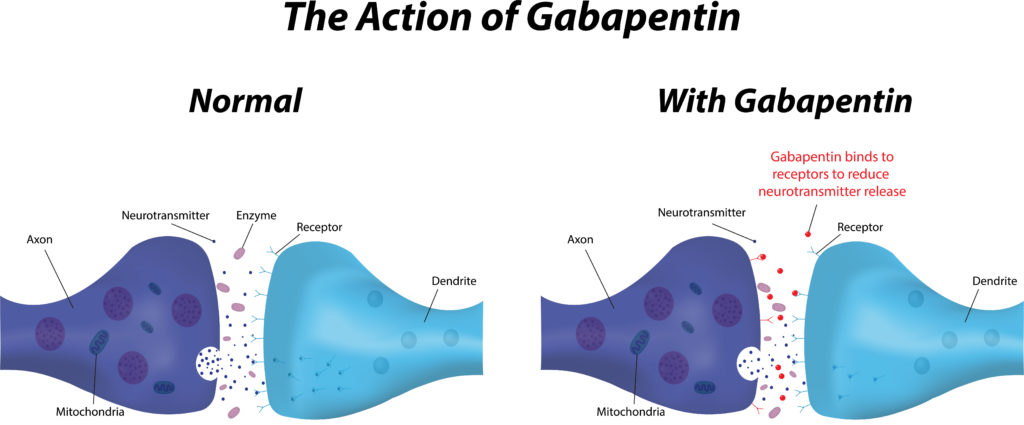 |
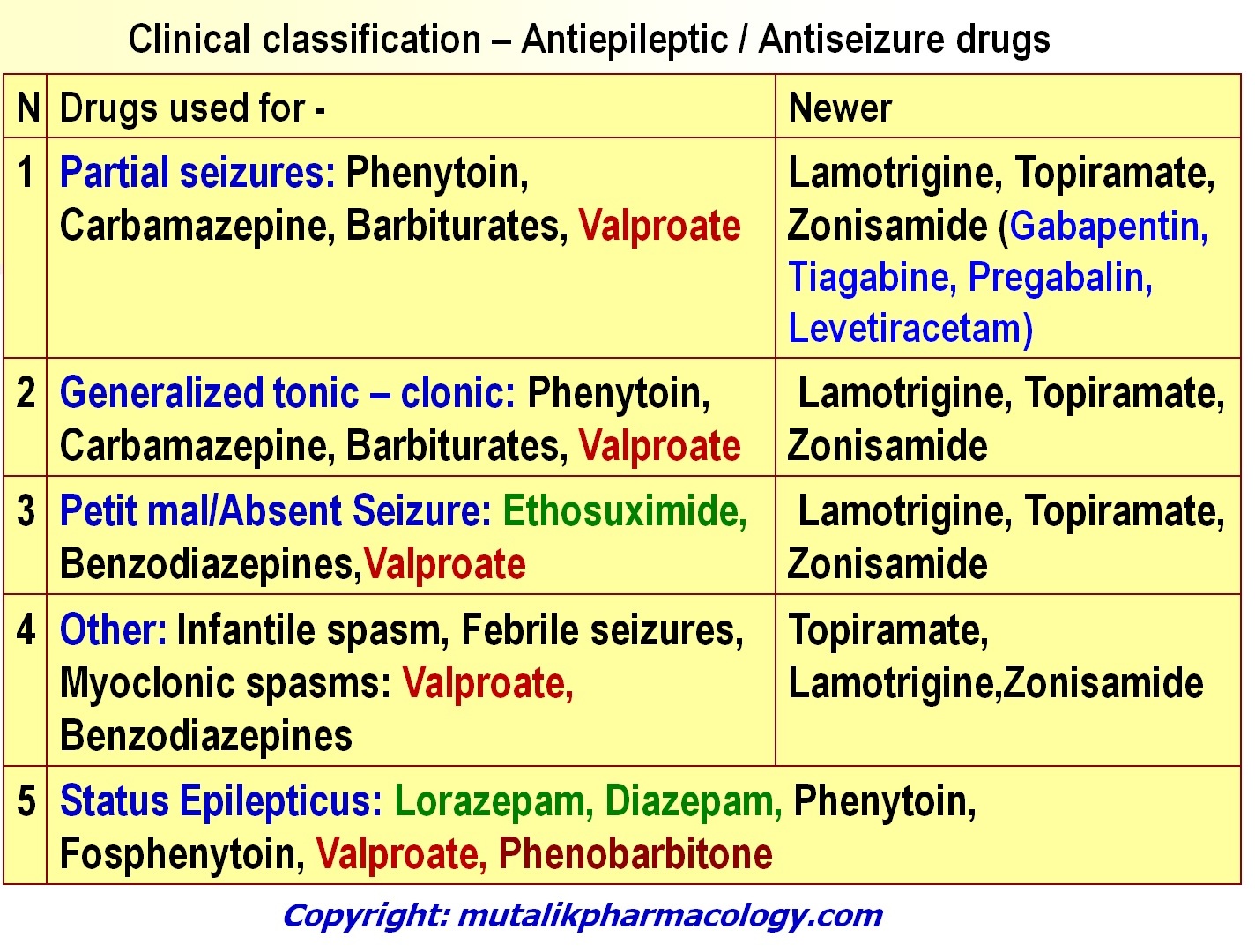
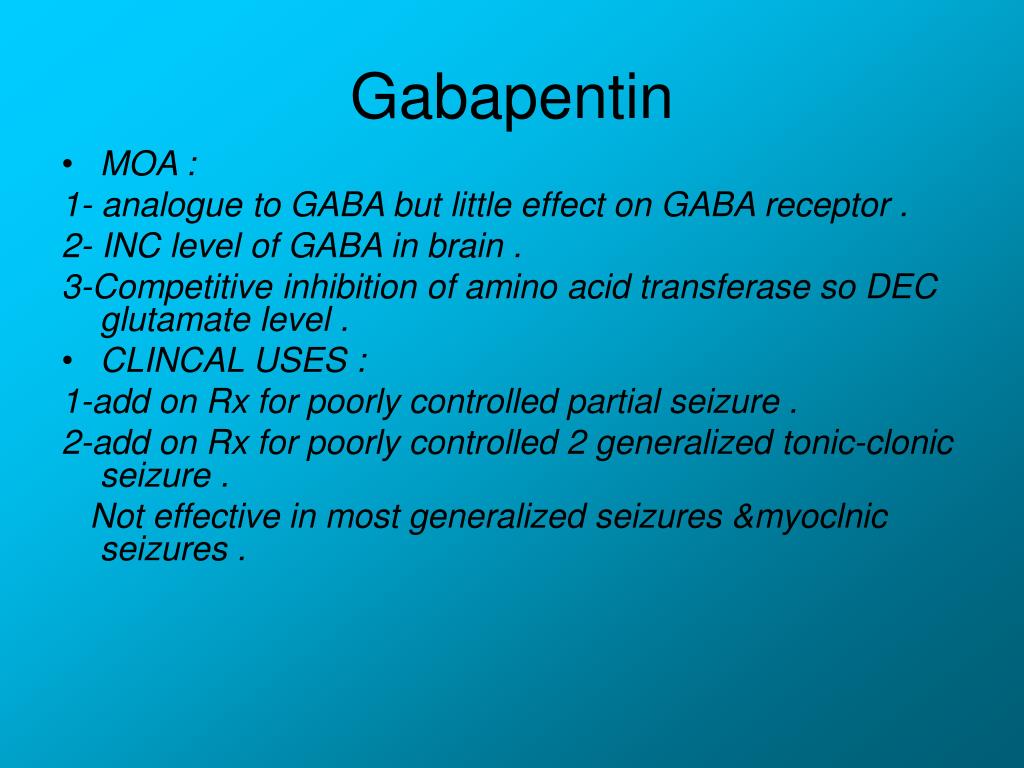
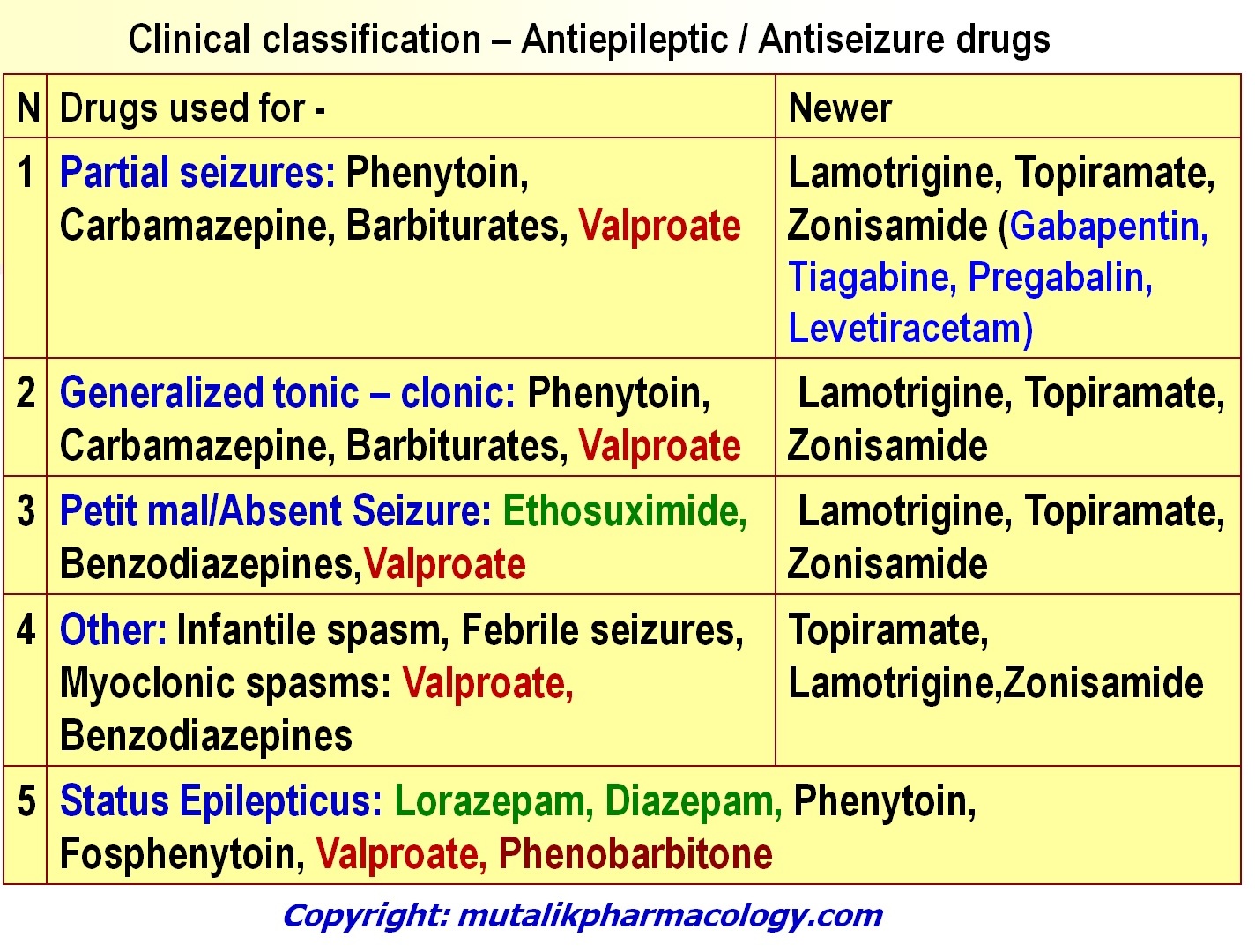
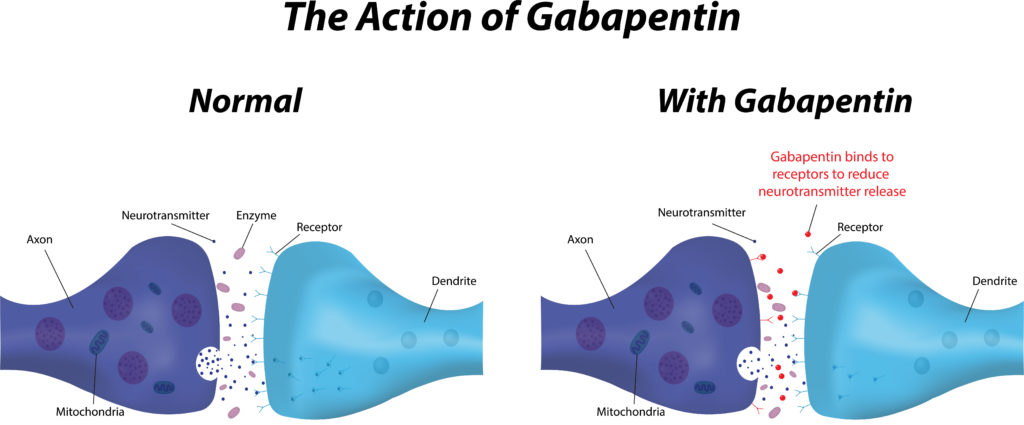
Synopsis Gabapentin is an antiepileptic drug with an unknown mechanism of action apparently dissimilar to that of other antiepileptic agents, and possessing some desirable pharmacokinetic traits. The drug is not protein bound, is not metabolised and does not induce liver enzymes, diminishing the likelihood of drug interactions with other antiepileptic agents and drugs such as oral Mechanism of Action. Gabapentin's exact mechanism of action is not fully understood, but it is believed to work by reducing abnormal electrical activity in the brain. It is thought to bind to calcium channels, modulating their activity and reducing the release of neurotransmitters involved in seizures and nerve pain. The International League Against Epilepsy (ILAE) recommended gabapentin as initial monotherapy of newly diagnosed, not yet treated focal seizures in adults; for focal seizures in the elderly; and for idiopathic focal epilepsy in children (Glauser 2006; Glauser 2013). Gabapentin is 1 of many antiseizure medications available for the treatment of epilepsy in adults; however, there are potential risks associated with its use. Therefore, it is important to determine the place of therapy of gabapentin in the treatment of epilepsy. Gabapentin (GBP) was approved on January 1994 as adjunctive treatment in patients 12 years or older with partial seizures, with or devoid of secondary generalization. Gabapentin prevents seizures in a wide variety of models in animals, including generalized tonic-clonic and partial seizures. Gabapentin has no activity at GABAA or GABAB receptors of GABA uptake carriers of brain. EEG shows spike and wave pattern at 3 Hz. The boy is started on ethosuximide. (Absence seizures) (AED) can be separated by mechanism of action (MOA) affecting It has a broad range of antiseizure activity in animal epilepsy models 100 including seizures induced by bicuculline, t-butylbicyclophosphorothionate (TBPS, a high affinity ligand for the GABA A R picrotoxin site), aminophylline and corneal kindling, and is well tolerated and effective against seizures in humans. Ganaxolone is currently under These neurons probably are an integral component of the thalamocortical circuits associated with absence seizures, a subtype of generalized seizures associated with brief episodes of staring and a characteristic three-per-second spike and wave pattern on the electroencephalogram (EEG) [1]. Gabapentin, sold under the brand name Neurontin among others, is an anticonvulsant medication primarily used to treat neuropathic pain and also for partial seizures [10] [7] of epilepsy. It is a commonly used medication for the treatment of neuropathic pain caused by diabetic neuropathy , postherpetic neuralgia , and central pain . [ 11 ] Gabapentin for partial seizures: According to the guidelines from the American Epilepsy Society, clinicians might consider gabapentin as a potential option for patients aged 60 and older with new-onset focal epilepsy, as it could be similarly effective and better tolerated compared to carbamazepine. Clinical trials and retrospective studies have consistently demonstrated the beneficial effects of gabapentin in reducing seizure frequency and improving overall seizure control. mechanism of action among currently available AEDs. The established agents phenytoin and carbamazepine are archetypal sodium channel blockers, a mechanism they share with the newer drugs, lamotrigine, felbamate, topiramate, oxcarbazepine, zonisamide, rufinamide, lacosamide, and eslicarbazepine acetate. Gabapentin is ineffective in absence seizures and should be used in caution in patients with mixed seizure disorders involving absence seizures. Gabapentin has been associated with drug reaction with eosinophilia and systemic symptoms (DRESS), otherwise known as multi-organ hypersensitivity. A 17-year-old man presents with myoclonic seizures followed by generalized a tonic-clonic seizure after awakening. He denies any recent head trauma or substance abuse. He reports to being sleep deprived for the past week due to final examinations. Routine EEG testing is significant for 5-Hz bilateral polyspike and slow wave discharges. Gabapentin increases the concentration and probably the rate of synthesis of GABA in brain, which may enhance non-vesicular GABA release during seizures. 3. Gabapentin binds with high affinity to a novel binding site in brain tissues that is associated with an auxiliary subunit of voltage-sensitive Ca2+ channels. Mechanism of action of gabapentin. The precise mechanism of action of gabapentin is not fully understood (Figure 8). However, it is believed to involve modulation of calcium channels and GABAergic neurotransmission in the central nervous system. Here is a simplified description of the proposed mechanism of action of gabapentin: Figure 8: Flow Max dosage 3600mg if patient already on gabapentin; Taper dose > 7 days to discontinue; Pediatric Dosing Partial seizures. Adjunct for partial seizures with out secondary generalization in patients> 12yo with epilepsy; also adjunctive therapy for partial seizures in patients 3-12 years <3 years: Safety and efficacy not established Discontinuation of therapy: In patients receiving gabapentin chronically, unless safety concerns require a more rapid withdrawal, gabapentin should be withdrawn gradually over ≥1 week to minimize the potential of increased seizure frequency (in patients with epilepsy) or other withdrawal symptoms (eg, confusion, irritability, tachycardia The transport of gabapentin across membranes and its demonstrated effects on voltage-gated ion channels (sodium, calcium), presynaptic mechanisms that can enhance GABAergic inhibition, and ligand-gated ion channels (GABA receptors and glutamate receptors) are reviewed.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |