Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 | |
 |  |
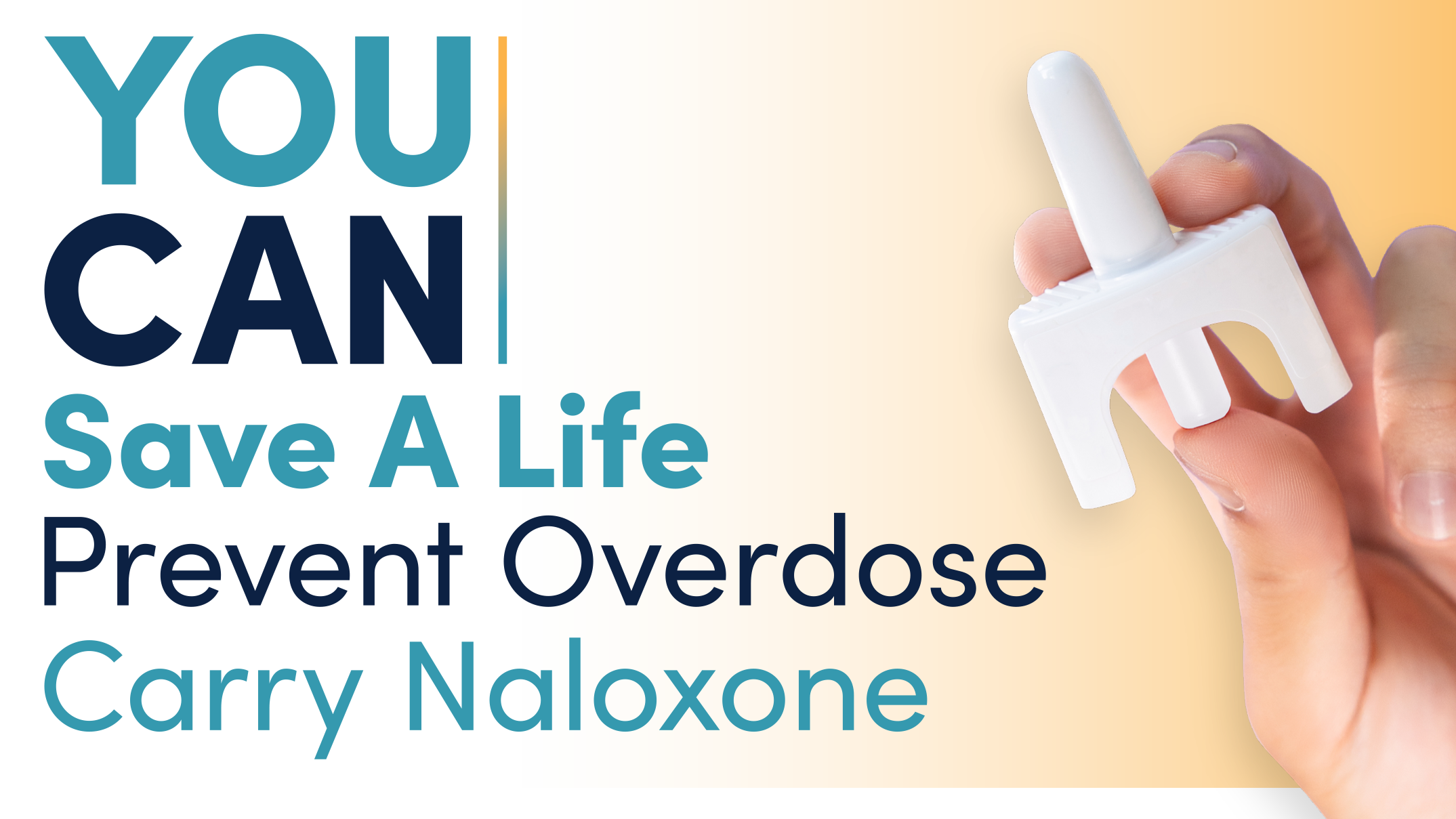
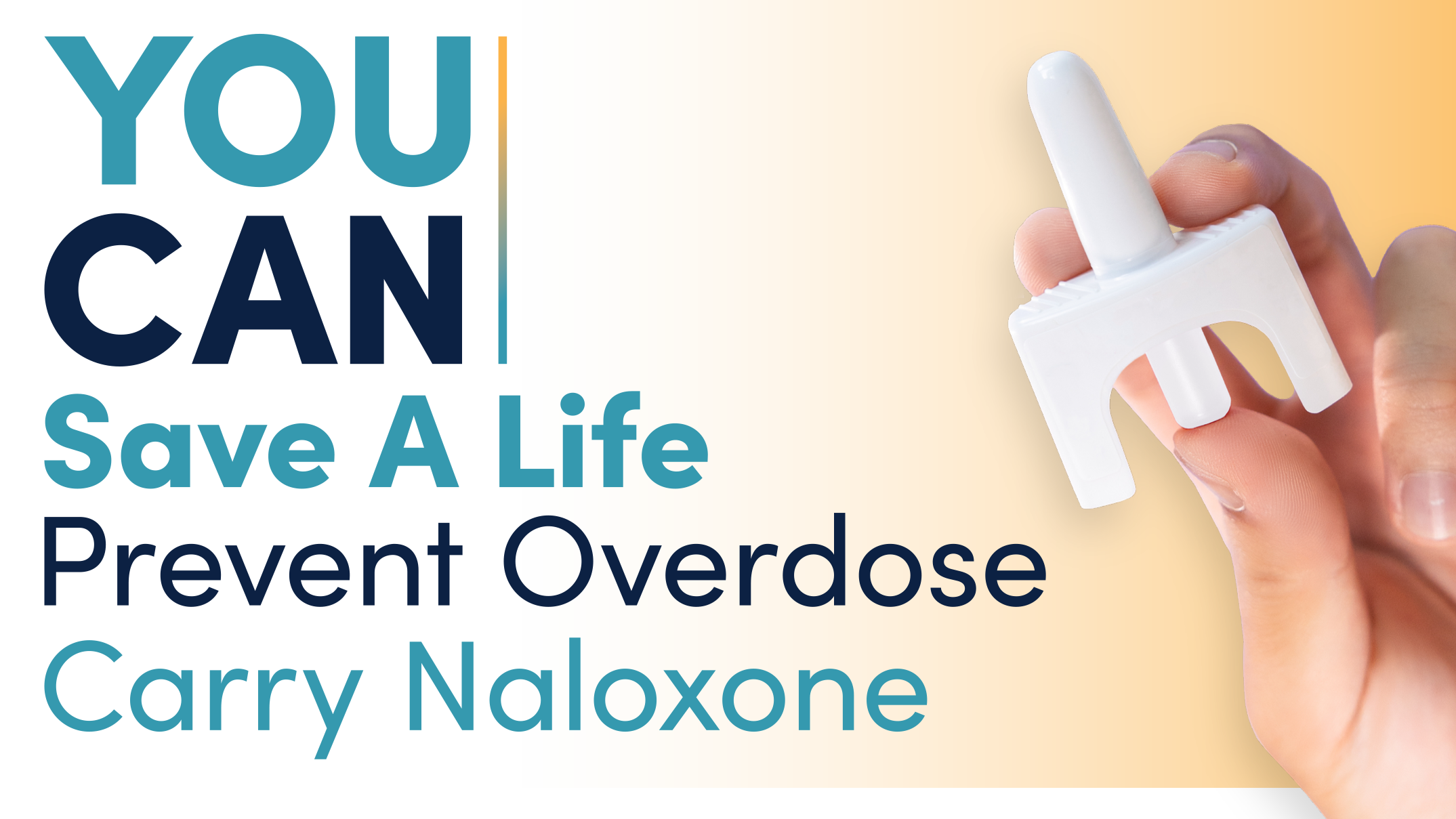
Overdose and Abuse. Even in large overdoses, gabapentin and pregabalin are usually well tolerated with only mild CNS depression and hypotension, unless there are co-ingestants involved. The risk of CNS depression is increased with opioids, benzodiazepines, barbiturates, and alcohol. One poison center review of gabapentin adverse effects described drowsiness, dizziness, tachycardia, ataxia, and hypotension; however, all cases were managed in an outpatient setting . These studies provide some understanding of individual anticonvulsants in overdose yet no direct comparison of newer anticonvulsants has been made. For healthcare professionals. Applies to gabapentin: compounding powder, oral capsule, oral solution, oral tablet, oral tablet extended release. General adverse events. The most common adverse reactions associated with the use of this drug were dizziness, somnolence, and peripheral edema. Gabapentinoids are commonly ingested in self-harm attempts and often misused for their sedative and euphoric properties. These medications can cause lethargy or agitation in overdose, increase risk of death combined with opioids, and manifest a withdrawal syndrome. Common neurological side effects of gabapentin include drowsiness, dizziness, and ataxia. Cases of hypoglycemia have been described in adult literature but not in pediatrics. Our patient exhibited drowsiness and hypotension, which may overlap with the signs of hypoglycemia. Signs & Symptoms of a Gabapentin Overdose. Gabapentin overdose symptoms include: Drowsiness; Slurred speech; Double vision; Lethargy/exhaustion; Diarrhea; Nausea and vomiting; Low blood pressure; Rapid heart rate; Labored breathing ; Marked sedation; Blue-colored skin, lips, fingers, and toes; Hypoactivity (inhibition of behavioral or locomotor Common symptoms of gabapentin overdose are drowsiness, fast heartbeat, dizziness, low blood pressure, nausea, vomiting, and impaired coordination. In severe cases, lethargy, coma, and death may occur. If someone takes too much gabapentin or takes gabapentin by accident, get guidance from Poison Control immediately. Gabapentin enacarbil available under the trade name Horizant is the only gabapentin product approved for treatment of Restless Legs Syndrome (RLS). A daily dose of 1200 mg provided no additional benefit compared with the 600 mg dose, but caused an increase in adverse reactions. Nine were symptomatic with reported effects of drowsiness (6), dizziness (3), nausea/vomiting (2), tachycardia (2), and hypotension (2). None of the patients were admitted for medical care. Conclusion: In this cases series, gabapentin exposures caused no or minimal toxicity. Fischer JH, Barr AN, Rogers SL, Fischer PA, Trudeau VL. Lack of serious toxicity following gabapentin overdose. Neurology 1994; 44(5):982-9833. Klein-Schwartz W, Shepherd JG, Gorman S et al. Characterization of gabapentin overdose using a poison center case series. Journal of Toxicology-Clinical Toxicology 2003; 41(1):11-15. Orthostatic hypotension (OH), defined as a reduction in systolic blood pressure (BP) of ≥20 mm Hg or diastolic BP of ≥10 mm Hg within 3 minutes of assuming an erect posture , is estimated to affect 30% to 70% of older adults and is commonly associated with use of medications . Gabapentin withdrawal symptoms have been reported since the drug was approved. However, the individuals in these reports experienced symptoms after discontinuing higher-than-recommended doses of gabapentin and for uses for which the drug was not approved. What’s known about gabapentin and overdose? Overdoses on gabapentin have been reported. Child 6–11 years 10 mg/kg once daily (max. per dose 300 mg) on day 1, then 10 mg/kg twice daily (max. per dose 300 mg) on day 2, then 10 mg/kg 3 times a day (max. per dose 300 mg) on day 3; usual dose 25–35 mg/kg daily in 3 divided doses, some children may not tolerate daily increments; longer intervals (up to weekly) may be more appropriate, daily dose maximum to be given in 3 divided We report a case of massive gabapentin and presumptive quetiapine overdose with the highest recorded serum gabapentin concentration (104.5 u/ml) associated with coma, respiratory depression requiring mechanical ventilation, and hypotension. Introduction. Orthostatic hypotension (OH) is an impaired blood pressure (BP) response to the upright position which is defined by a systolic BP drop ≥ 20 mmHg or by an absolute systolic BP value ≤ 90 mmHg and/or a diastolic BP drop ≥ 10 mmHg within 3 minutes of standing [1, 2]. - pregabalin/gabapentin naive Seizures - Benzodiazepines: Diazepam 5mg IV (Paediatric 0.2 mg/kg IV) every 5 minutes as necessary Clinical features: Hypotension Gabapentin does not undergo metabolism and is excreted in the urine as unchanged drug . Pathophysiology of Toxic Effects. The toxic effects of clinically significant gabapentin overdose include lethargy, ataxia, central nervous system (CNS) depression, hypotension, bradycardia, tachycardia, and dizziness [1, 6]. Driving performance studies conducted with a prodrug of gabapentin (gabapentin enacarbil tablet, extended-release) indicate that gabapentin may cause significant driving impairment. Prescribers and patients should be aware that patients' ability to assess their own driving competence, as well as their ability to assess the degree of somnolence Gabapentin and pregabalin are structurally similar to gamma aminobutyric acid (GABA) but have little to no activity on the GABAergic system. Instead, they inhibit the α 2-δ subunit of P/Q-type voltage-gated calcium channels, thereby reducing presynaptic calcium influx and thus subsequent release and activity of excitatory neurotransmitters such as glutamate and substance P. 9 Gabapentin was Anyone who shows signs of an overdose or allergic reaction to gabapentin should contact emergency medical services immediately. Left untreated, these symptoms can turn fatal. Treatment for Gabapentin Overdose
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 | |
 |  |