Gallery
Photos from events, contest for the best costume, videos from master classes.
 | |
 |  |
 |  |
 |  |
 | |
 | 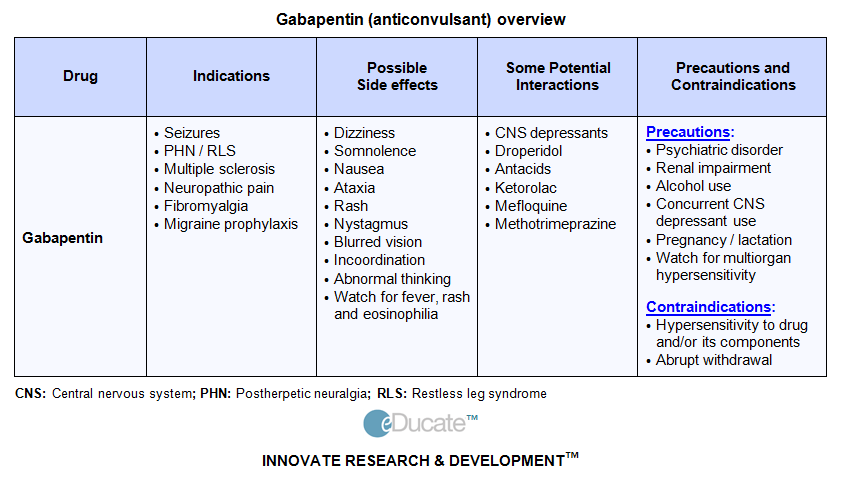 |
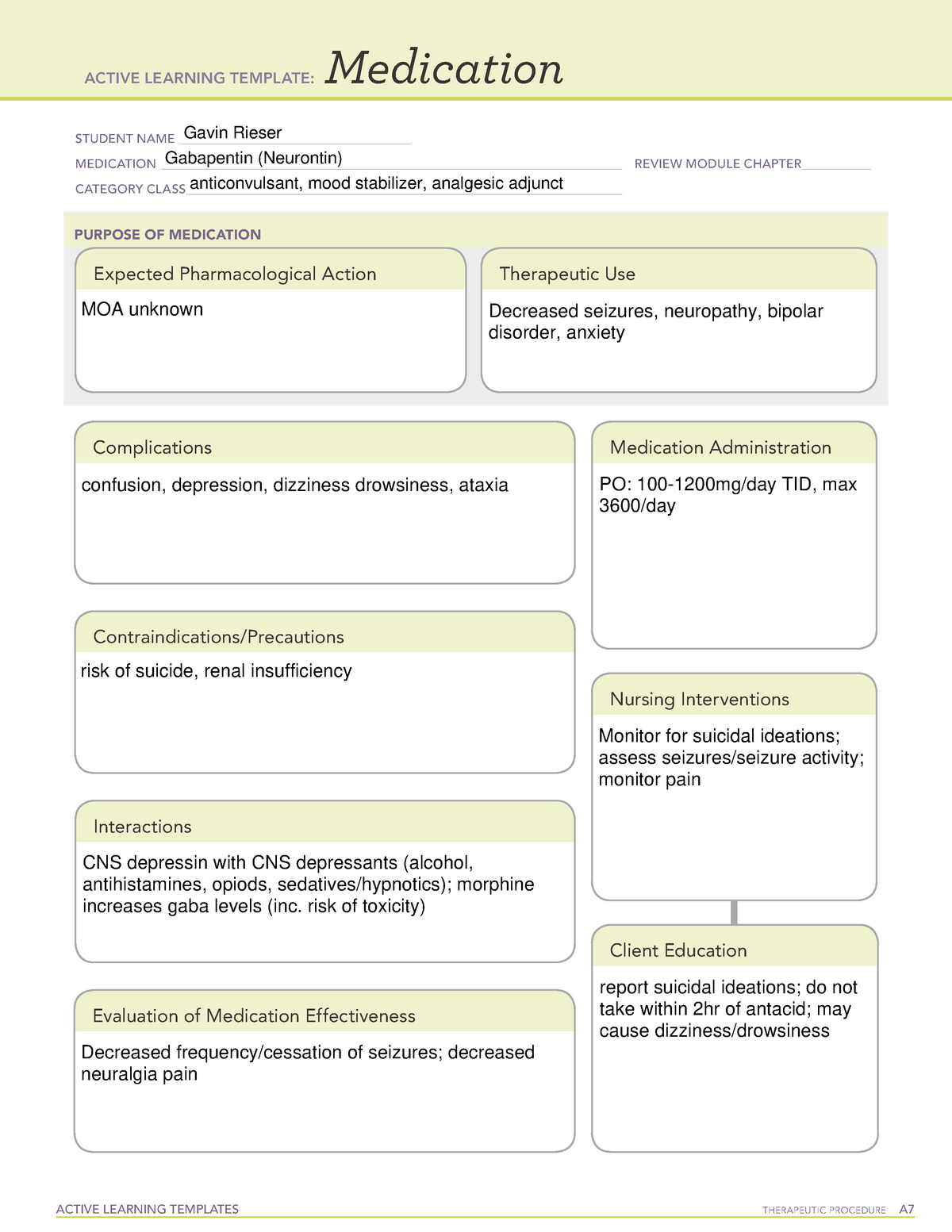
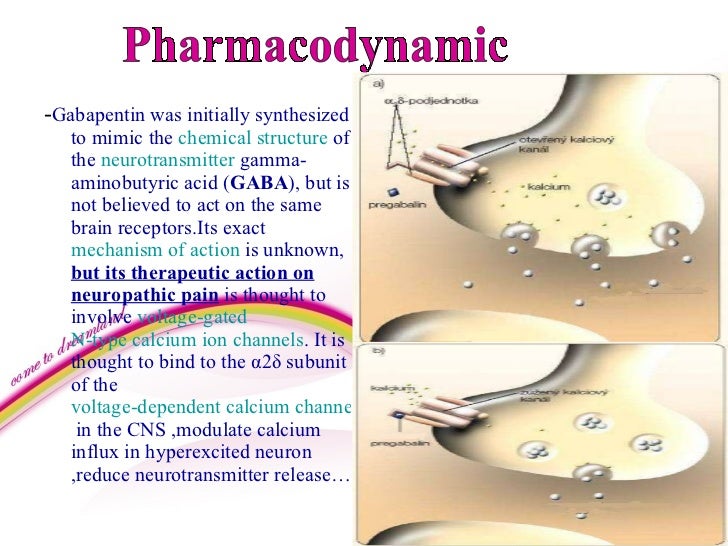
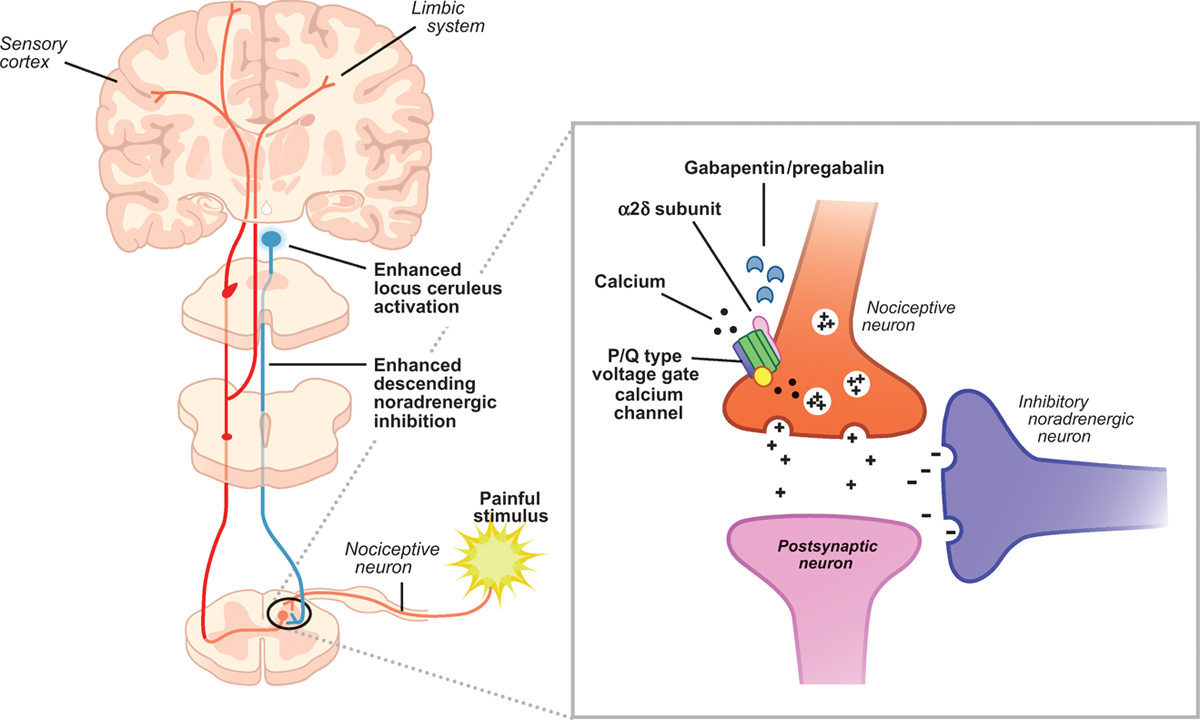
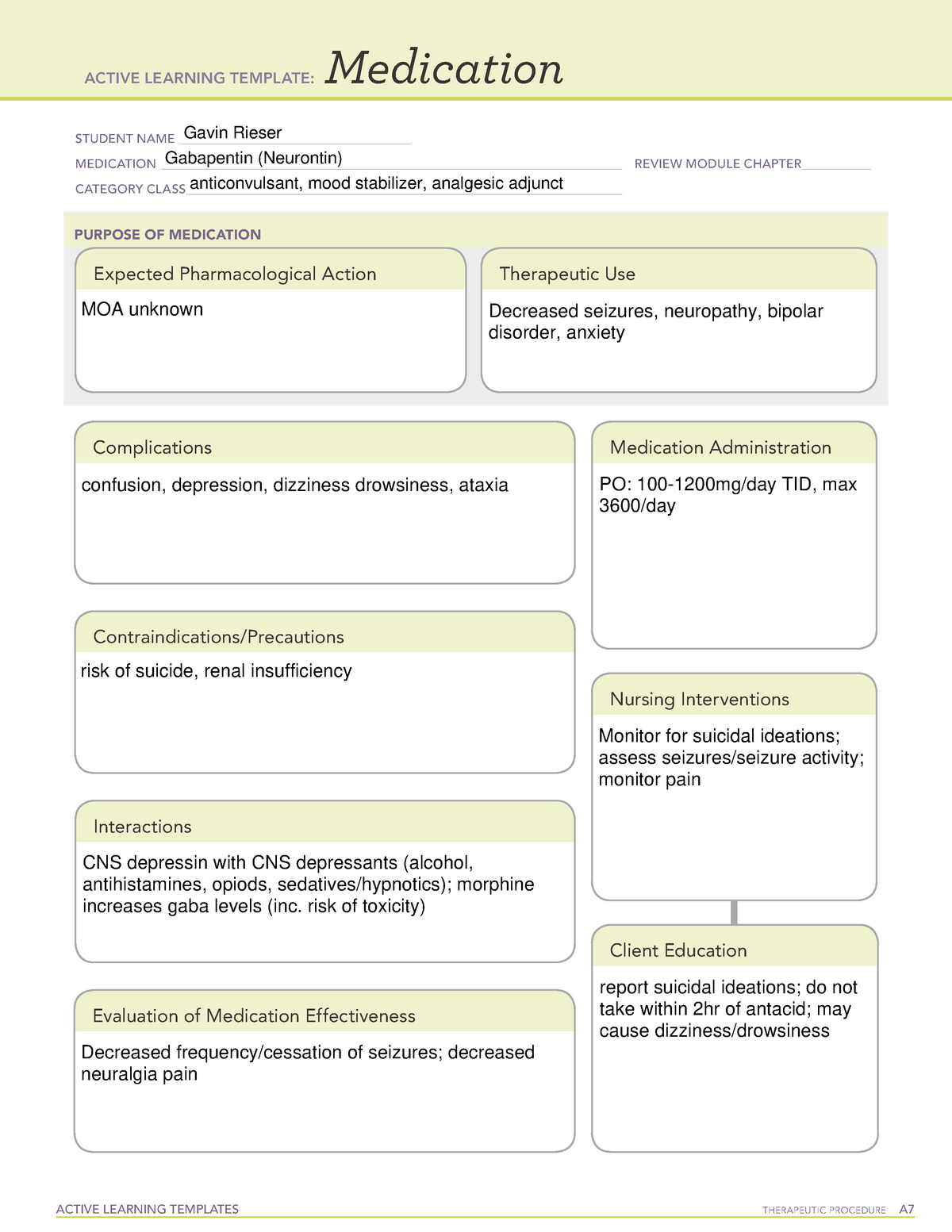
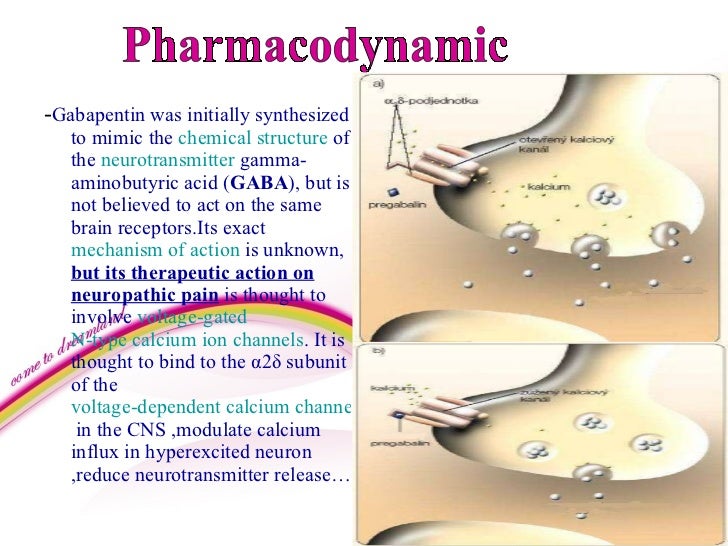
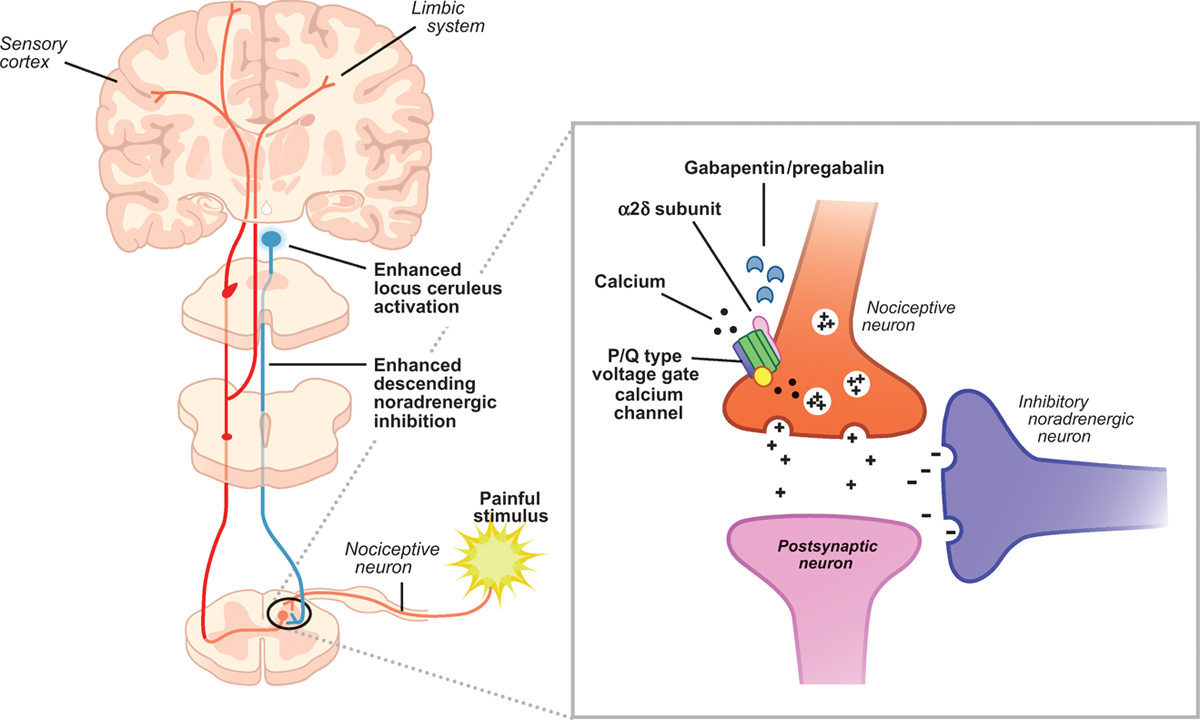
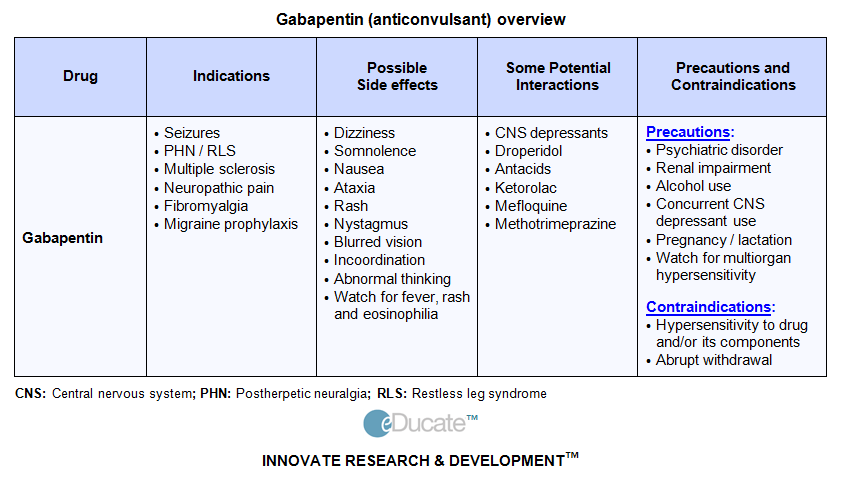
Gabapentin is an anti-epileptic agent but now it is also recommended as first line agent in neuropathic pain, particularly in diabetic neuropathy and post herpetic neuralgia. α2δ-1, an auxillary subunit of voltage gated calcium channels, has been documented as its main target and its specific binding to this subunit is described to produce different actions responsible for pain attenuation Gabapentin: Gabapentin is indicated for postherpetic neuralgia and serves as adjunctive therapy for managing partial seizures (with or without secondary generalization) in adults and pediatric patients aged 3 or older. Gabapentin is an anticonvulsive medication that received approval from the US Food and Drug Administration (FDA) in 1993 and has been available in generic form in the USA since 2004. Gabapentin was originally used as a muscle relaxant and an anti-spasmodic. However, it was later discovered that gaba Gabapentin has no direct GABAergic action and does not block GABA uptake or metabolism. Gabapentin blocks the tonic phase of nociception induced by formalin and carrageenan, and exerts a potent inhibitory effect in neuropathic pain models of mechanical hyperalgesia and mechanical/thermal allodynia. Gabapentin is an anti-epileptic drug but its use has expanded to treat multiple other diseases including post-herpetic neuralgia, neuropathic pain, and spasticity. The mechanism of action is not fully understood but may be related to gabapentin’s action on calcium channels leading to diminution of excitatory neurotransmitters. Gabapentin Mechanism of action. Gabapentin does not act directly on GABA receptors in spite of their close structural resemblance to GABA. They may, however, modify the synaptic or nonsynaptic release of GABA. An increase in brain GABA concentration is observed in patients receiving gabapentin. Mechanism of action: By inhibiting the voltage-gated calcium channels in the CNS, gabapentin reduces the release of excitatory neurotransmitters (mostly noradrenaline, dopamine and serotonin), and therefore decreases epileptogenesis. Clinical effects Mechanism of action of gabapentinoids Site of action The actions of gabapentinoids are mainly at an intracellular site and require active uptake.21 They were originallydesigned as g aminobutyric acid (GABA) analogues but do not have any effects on GABA receptors. Gabapentin binds to a 2d receptors with greater affinity to the a 2d-1 subtype.22 Gamma-aminobutyric acid (GABA) and glutamate (GLU) play crucial roles in the control of neuropathic pain through their actions within the central nervous system (CNS). These neurotransmitters separately activate two distinct classes of receptors: ionotropic and metabotropic. Gabapentin is effective as monotherapy for partial seizures (Beydoun 1999).However, although few studies have compared the effectiveness of gabapentin with other AEDs in the management of partial epilepsy, available evidence suggests that monotherapy with gabapentin is less effective than traditional agents such as carbamazepine and the newer antiepileptic drug lamotrigine (Marson et al. 2007). The past 15 years has witnessed the unprecedented development of novel antiepileptic agents [1].One of the first compounds to emerge from this era was gabapentin (GBP), which was licensed for the treatment of refractory localisation-related epilepsies in the UK and Europe in 1993. Gabapentin crosses several lipid membrane barriers via system L amino acid transporters. In vitro, gabapentin modulates the action of the GABA synthetic enzyme, glutamic acid decarboxylase (GAD) and the glutamate synthesizing enzyme, branched-chain amino acid transaminase. I appreciate the comments of Gazulla et al. regarding my focused review on the mechanisms of action and side effects of gabapentinoids. 1 I cited the article by Yu et al., as they found that gabapentin increases expression of delta subunit-containing GABAA receptors. 2 I am also aware of the placebo-controlled pilot study of Gazulla et al. regarding the potential benefit of pregabalin for Gabapentin is an anti-convulsant medication that inhibits the release of excitatory neurotransmitters, allowing for its use against pathologic neurotransmission such as that seen in neuropathic pain and seizure disorders. 16,19 It has a wide therapeutic index, with doses in excess of 8000 mg/kg failing to cause a fatal reaction in rats. 21 Gabapentin is not appreciably metabolized in humans. Gabapentin elimination half-life is 5 to 7 hours and is unaltered by dose or following multiple dosing. Gabapentin elimination rate constant, plasma clearance, and renal clearance are directly proportional to creatinine clearance. Mechanisms of action. Gabapentin and pregabalin do not bind to GABA receptors despite their structural similarity but have a high affinity for the α2δ-1 subunit of voltage-gated calcium channels (VGCCs). 19 VGCCs are composed of multiple subunits: α 1, β, γ and α 2 δ. Gabapentin is regarded as safe and tolerable with a promising pharmacokinetic profile and an extensive therapeutic index. 10 Also, gabapentin have been approved in Japan as adjunctive drug therapy for medically intractable seizures. 4 Gabapentin is an anti-epileptic agent but now it is also recommended as first line agent in neuropathic pain, particularly in diabetic neuropathy and post herpetic neuralgia. α2δ-1, an auxillary subunit of voltage gated calcium channels, has been documented as its main target and its specific bindin Gabapentin is an amino acid that exists at physiological pH as a zwitterion, and since it is doubly-charged, its native permeability to membrane barriers within the body is low. It discusses gabapentin's mechanism of action, approved uses, dosing, pharmacokinetics, interactions, adverse effects and overdose treatment. It then summarizes a clinical study comparing the dose-response relationship of pregabalin and gabapentin in patients with partial seizures, finding that pregabalin was more potent and effective at
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 | |
 |  |
 |  |
 |  |
 | |
 |  |