Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
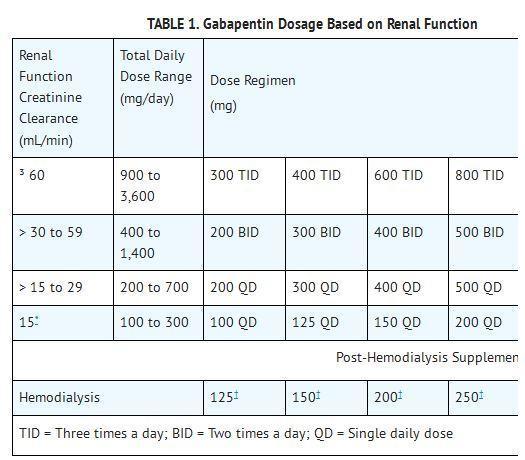
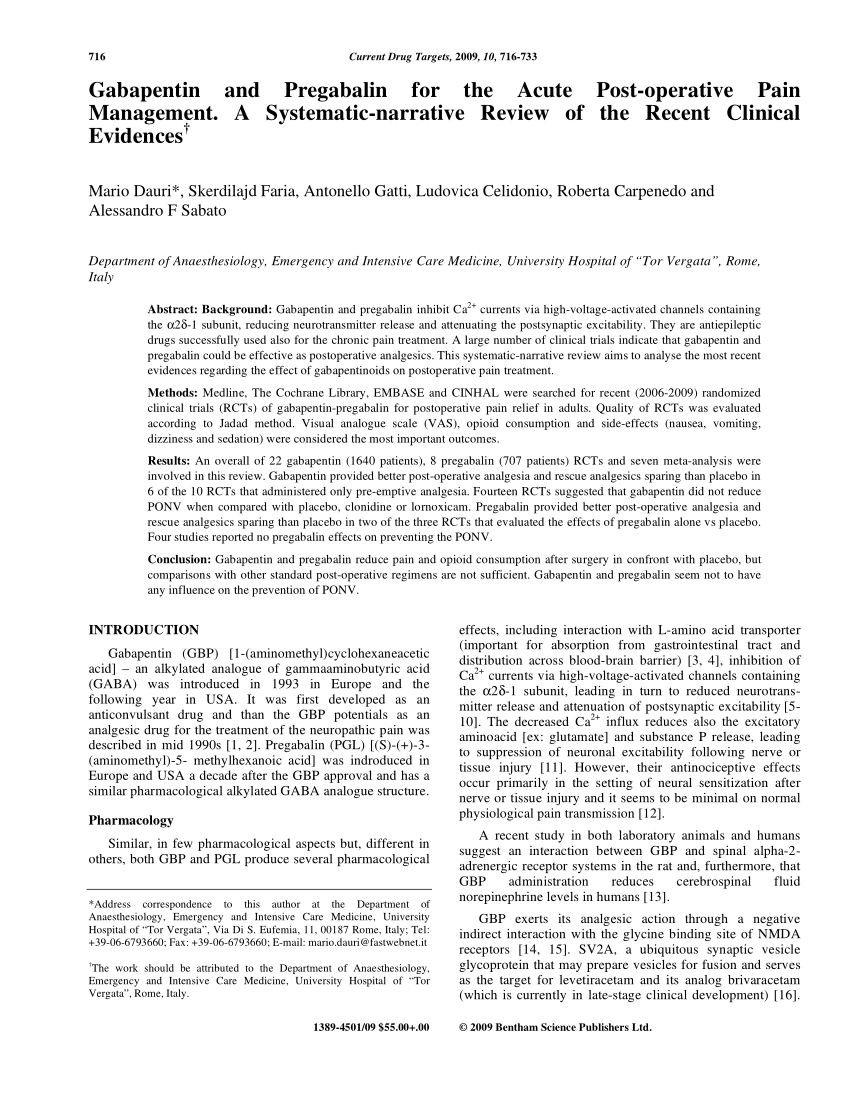
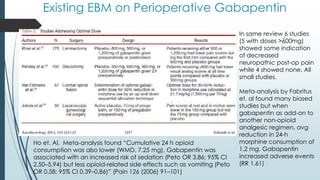
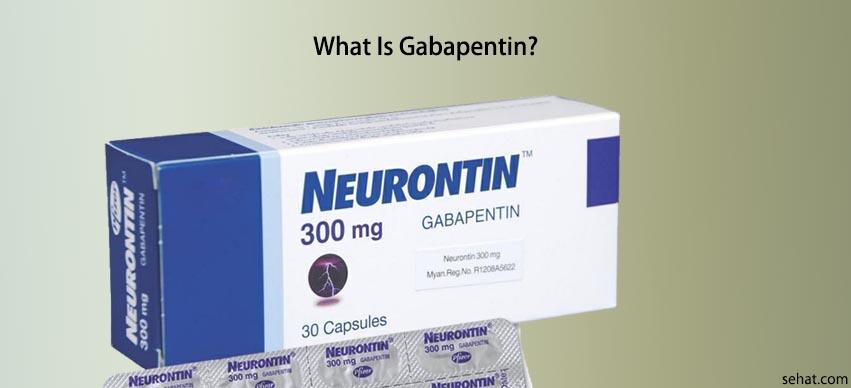
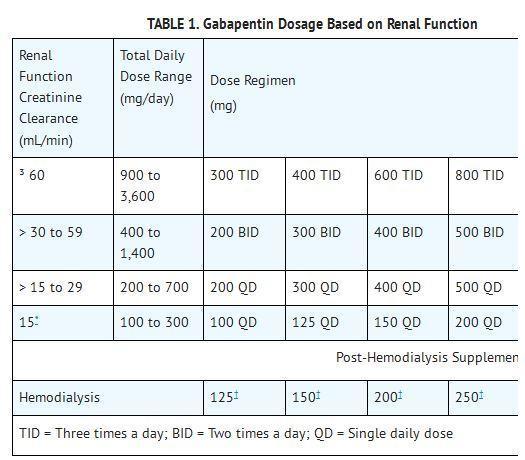
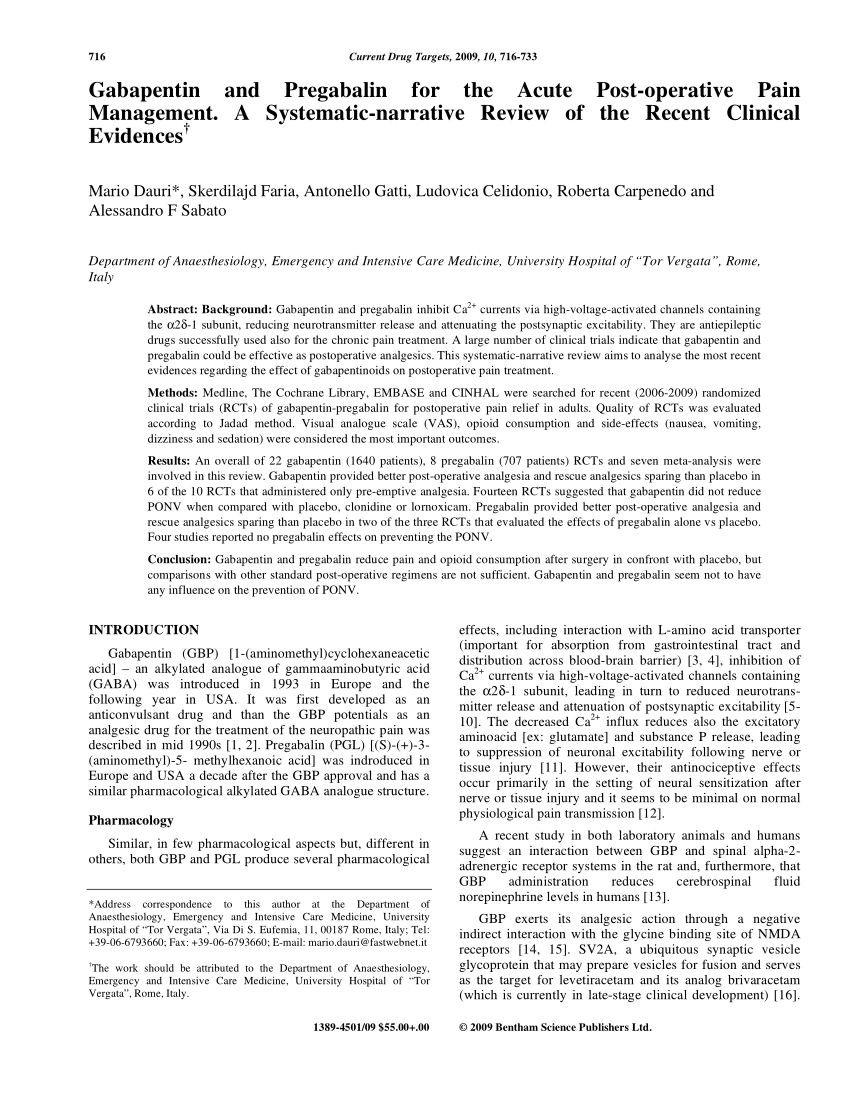
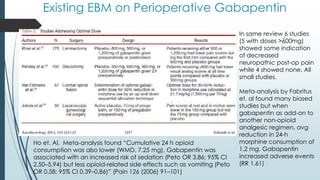
Background Gabapentin is an antiepileptic drug used in a variety of chronic pain conditions. Increasing numbers of randomized trials indicate that gabapentin is effective as a postoperative analgesic. This procedure-specific systematic review aims to analyse the 24-hour postoperative effect of gabapentin on acute pain in adults. Methods Medline, The Cochrane Library and Google Scholar were Randomised placebo-controlled trials (RCTs) investigating peri-operative gabapentin for post-operative pain management were eligible for inclusion. Eligible outcomes were relevant pain outcomes such as pain scores, time to first analgesic request and post-operative cumulative opioid consumption. First, we repeated the analysis by defining gabapentin exposure on the day of surgery without requiring a 2-day minimum length of stay after surgery. Then, we explored a dose-response relationship using a 4-dose category of gabapentin (no use, 1 mg to <600 mg, 600 mg to <1200 mg, or ≥1200 mg). The prevalence of prolonged use of post-operative gabapentin among older adults is unknown, as are the factors associated with prolonged use. Finally, the incidence of prolonged use in conjunction with opioids, a combination found to lead to serious adverse events including overdose and death, 11 , 12 has not been studied. Gabapentin is an anticonvulsant medication but demonstrates benefits in neuropathic and chronic pain. 28 In patients undergoing ambulatory hand procedures, preoperative gabapentin was shown to reduce postoperative pain medication consumption significantly and prolong the time to the patient’s first postoperative pain medication request versus Gabapentin is a novel drug used for the treatment of postoperative pain with antihyperalgesic properties and a unique mechanism of action, which differentiates it from other commonly used drugs. Various studies have shown that perioperative use of gabapentin reduces postoperative pain. The administration of gabapentin is effective in decreasing postoperative narcotic consumption and the VAS score. Keywords: Gabapentin, Total hip arthroplasty, Meta-analysis. Background. Total hip arthroplasty (THA) is a common and successful surgery in modern medicine, but it is often associated with intense postoperative pain . Pre-emptive A recent systematic review of randomized controlled trials (RCTs) reported that both gabapentin and pregabalin were efficacious in the management of postoperative pain in the immediate post-operative period. 46 Khurana et al demonstrated that pregabalin is associated with less pain intensity and improved functional outcomes three months after A guideline for the use of gabapentin as part of a multi-modal pain management strategy for acute pain. It reviews the evidence, recommendations, and side effects of gabapentin dosing pre- and post-operatively. Would you want to take Lyrica (pregabalin) or Neurontin (gabapentin) for pain relief after a major surgery? Both drugs belong to a class of nerve medication called gabapentinoids that are increasingly being prescribed to patients perioperatively (after surgery) as an alternative to opioid medication. Gabapentin, an anticonvulsant, has recently been suggested as an effective postoperative ‘analgesic’ agent. The objective of the present study was to examine the analgesic effectiveness, opioid-sparing effects and side effects associated with the use of gabapentin in a perioperative setting. Gabapentin appears safe and well tolerated when used for persistent post-operative and post-traumatic pain in thoracic surgery patients, although minor side effects do occur. Gabapentin may relieve refractory chest wall pain in some of these patients, particularly those with more severe pain. In summary, the administration of gabapentin was effective in decreasing postoperative narcotic consumption and the incidence of pruritus. There was a high risk of selection bias and a higher heterogeneity of knee flexion range in this analysis. Gabapentin 250 mg is statistically superior to placebo in the treatment of established acute postoperative pain, but the NNT of 11 for at least 50% pain relief over 6 hours with gabapentin 250 mg is of limited clinical value and inferior to commonly used analgesics. The purpose of this review is to critically appraise the evidence for the use of gabapentinoids for acute pain management and its impact on the development of chronic pain after surgery. Recent findings: Recent meta-analyses have revealed that prior data likely have overestimated the beneficial effects of gabapentinoids in acute perioperative In response to the opioid crisis, surgeons nationwide have sought to decrease opioid use by adopting opioid-sparing multimodal medication regimens to treat perioperative pain. 1 For example, gabapentinoids (gabapentin and pregabalin) are now commonly administered during the perioperative period as part of “enhanced recovery after surgery Pre-operative gabapentin does not decrease long-term narcotic use and is associated with increased side effects of respiratory depression, sedation, and falls. Post-operative gabapentin (600 mg) may be equally effective as a preoperative dose in decreasing PACU narcotic use. • Level 3 The aim was to document beneficial and harmful effects of perioperative gabapentin treatment. Methods: Randomized clinical trials comparing gabapentin vs. placebo or active placebo in adult surgical patients receiving gabapentin perioperatively were included. Perioperative gabapentin, 1200 mg, administered preoperatively plus 600 mg every 8 hours continued for 72 hours after surgery did not affect time to pain cessation, the rate of pain resolution, or the proportion of patients with chronic pain at 6 months or 1 year following surgery. Gabapentin After Surgery Ups Risks in Older Adults Delirium incidence in this study was lower than previously reported post-surgery incidences of 15% to 25% due to the low sensitivity and high
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |