Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 | |
 |  |
 |  |
 |  |
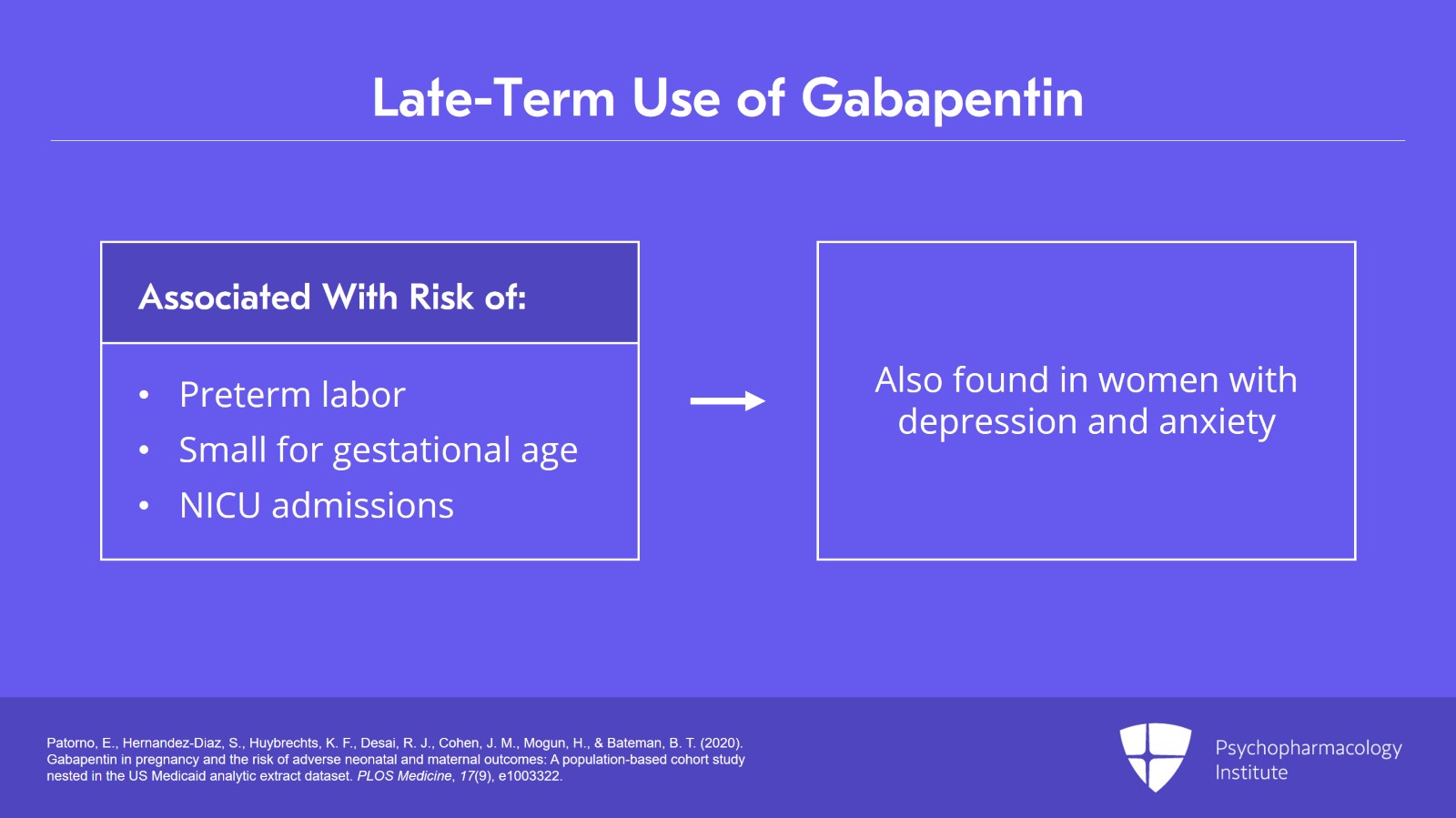
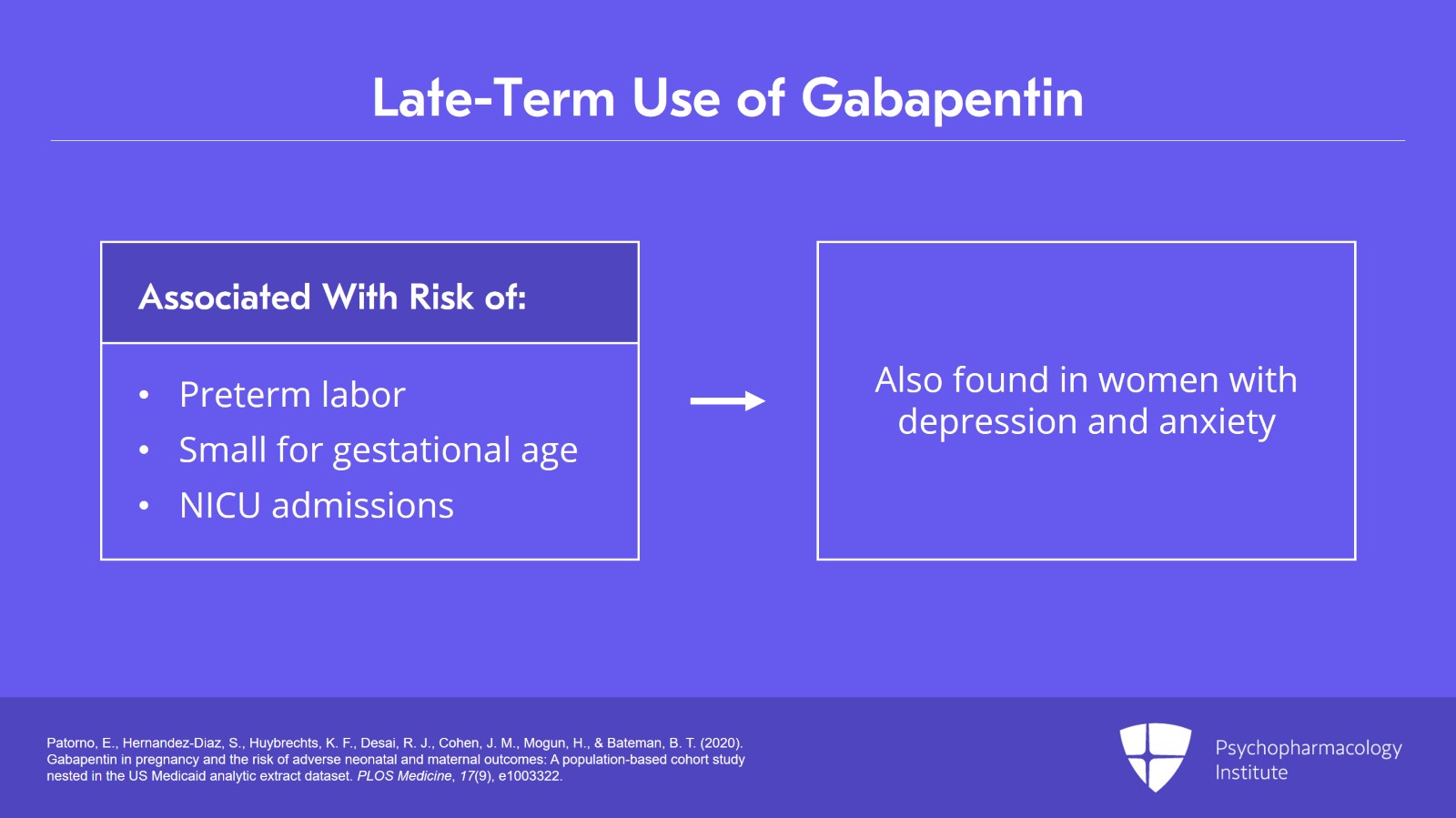
When treating neuropathic pain in a woman who is pregnant, the use of gabapentinoids (e.g. gabapentin) or an antiepileptic drug (AED) (e.g. levetiracetam, lamotrigine) is a last line option. This is due to the limited availability of data for safe use during pregnancy. Other options should be trialled first. Gabapentin (Neurontin®) is mainly used to treat epilepsy and nerve pain, and to prevent migraine. What are the benefits of taking gabapentin in pregnancy? Gabapentin prevents epileptic seizures, which can be dangerous to the woman and also lead to pregnancy complications. Pregnancy-related problems, such as preterm delivery (birth before week 37) or low birth weight (weighing less than 5 pounds, 8 ounces [2500 grams] at birth) have been reported in some studies looking at the use of gabapentin during pregnancy. Gabapentin/first trimester of pregnancy: 10 newborns (0.01%) [30] Patorno et al., 2020: Gabapentin/first trimester of pregnancy: 4642 pregnancies (0.26%) Patorno et al., 2020: Gabapentin/early in pregnancy (first 140 days of pregnancy and no gabapentin dispensing from the 141 and 245 days)3745 pregnancies (0.21%) Patorno et al., 2020 Advice and warnings for the use of Gabapentin during pregnancy. FDA Pregnancy Category C - Risk cannot be ruled out Amitriptyline is quite commonly used in pregnancy, whereas duloxetine, gabapentin and pregabalin are less commonly used to treat pain in pregnancy. When deciding which medicine to use, your doctor will help you to weigh up the benefits of each treatment against any possible risks to you and your baby. Pregnancy-related problems, such as preterm delivery (birth before week 37) or low birth weight (weighing less than 5 pounds, 8 ounces [2500 grams] at birth) have been reported in some studies looking at the use of gabapentin during pregnancy. Use of gabapentin in pregnancy may sometimes be considered necessary to control epilepsy or neuropathic pain. Your doctor or specialist will help you make decisions about your treatment. Gabapentin may cause side effects such as dizziness, drowsiness, and dizziness. It is important to follow the prescribed dosage and seek medical attention if experiencing serious side effects or changes in mood or behavior. Gabapentin is prescribed by healthcare professionals and should only be taken under medical supervision. All pregnant women in the UK will be offered a very detailed anomaly scan at around 20 weeks of pregnancy as part of their routine antenatal care. No extra monitoring for major birth defects is required following gabapentin use in pregnancy. Babies exposed to gabapentin before delivery may experience withdrawal symptoms for a few days after birth. If you're trying to get pregnant or have become pregnant while taking gabapentin, it is recommended to take a high dose of folic acid (5mg a day). You can get this from your doctor or midwife. Ideally you'll take high dose folic acid for 3 months before you start trying to get pregnant and for the first 12 weeks of pregnancy. Gabapentin should only be used during pregnancy where benefits of treatment are considered to outweigh any potential risks. In view of the limited human pregnancy data, close monitoring of mother and fetus should be considered with use of gabapentin in pregnancy. We have data on 223 pregnancy outcomes exposed to gabapentin and 223 unexposed pregnancies. The rates of major malformations were similar in both groups (p = 0.845). There was a higher rate of preterm births (p = 0.019) and low birth weight <2,500 g (p = 0.033) in the gabapentin group. For more information, please see the bump leaflet on Topiramate. Gabapentin, venlafaxine, and botulinum toxin are only used in pregnancy to prevent migraine if other medicines have not worked or cannot be used. They are not known to harm the developing baby but more information on their pregnancy safety is ideally required. For more information, please see the bump leaflet on Topiramate. Gabapentin, venlafaxine, and botulinum toxin are only used in pregnancy to prevent migraine if other medicines have not worked or cannot be used. They are not known to harm the developing baby but more information on their pregnancy safety is ideally required. Child 6–11 years 10 mg/kg once daily (max. per dose 300 mg) on day 1, then 10 mg/kg twice daily (max. per dose 300 mg) on day 2, then 10 mg/kg 3 times a day (max. per dose 300 mg) on day 3; usual dose 25–35 mg/kg daily in 3 divided doses, some children may not tolerate daily increments; longer intervals (up to weekly) may be more appropriate, daily dose maximum to be given in 3 divided A meta-analysis by Veroniki et al 2017a also did not suggest an increased risk of overall major congenital malformation with gabapentin use during pregnancy. However, gabapentin was found to be We examined the risk of major congenital malformations and cardiac defects associated with gabapentin exposure during the first trimester (T1), and the risk of preeclampsia (PE), preterm birth (PTB), small for gestational age (SGA), and neonatal intensive care unit admission (NICUa) associated with gabapentin exposure early, late, or both early If you have an unplanned pregnancy while taking a medicine, you should tell your doctor as soon as possible. If a new medicine is suggested for you during pregnancy, please make sure that the person prescribing it knows that you are pregnant. If you have any concerns about a medicine, you can check with your doctor, midwife or pharmacist. Bumps (Best Use of Medicines in Pregnancy) has been designed to provide freely available, reliable, evidenced-based and accurate information about the use of medicines in pregnancy. Our aim is to help women make decisions regarding use of medicines in pregnancy that are best for both mother and baby.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 | |
 |  |
 |  |
 |  |