Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
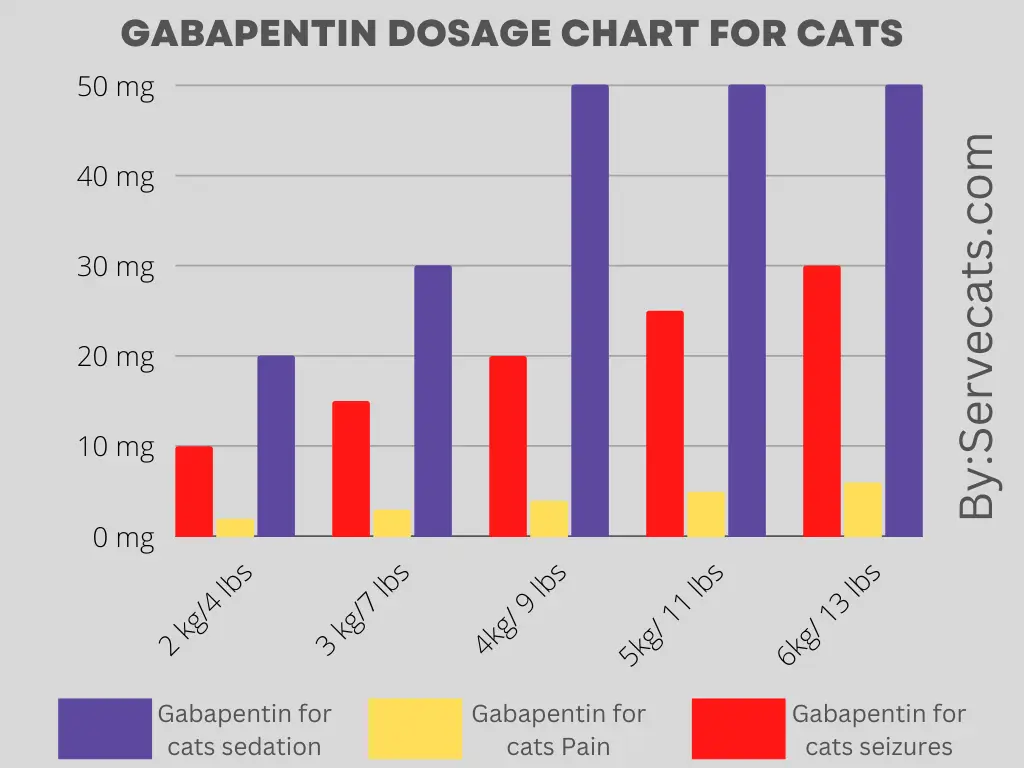
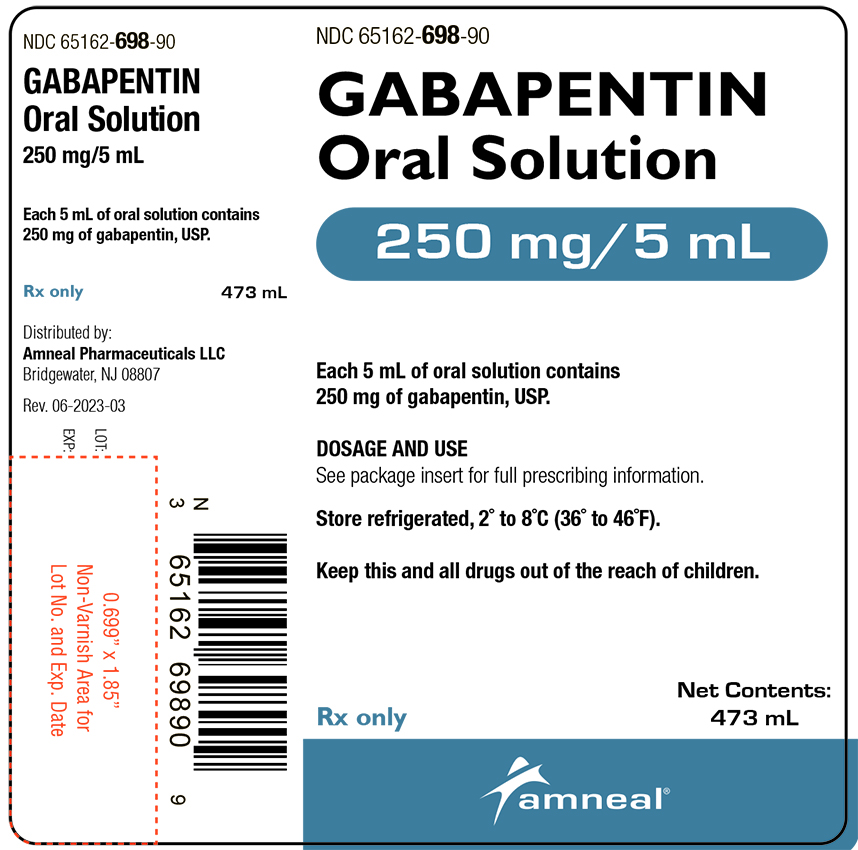
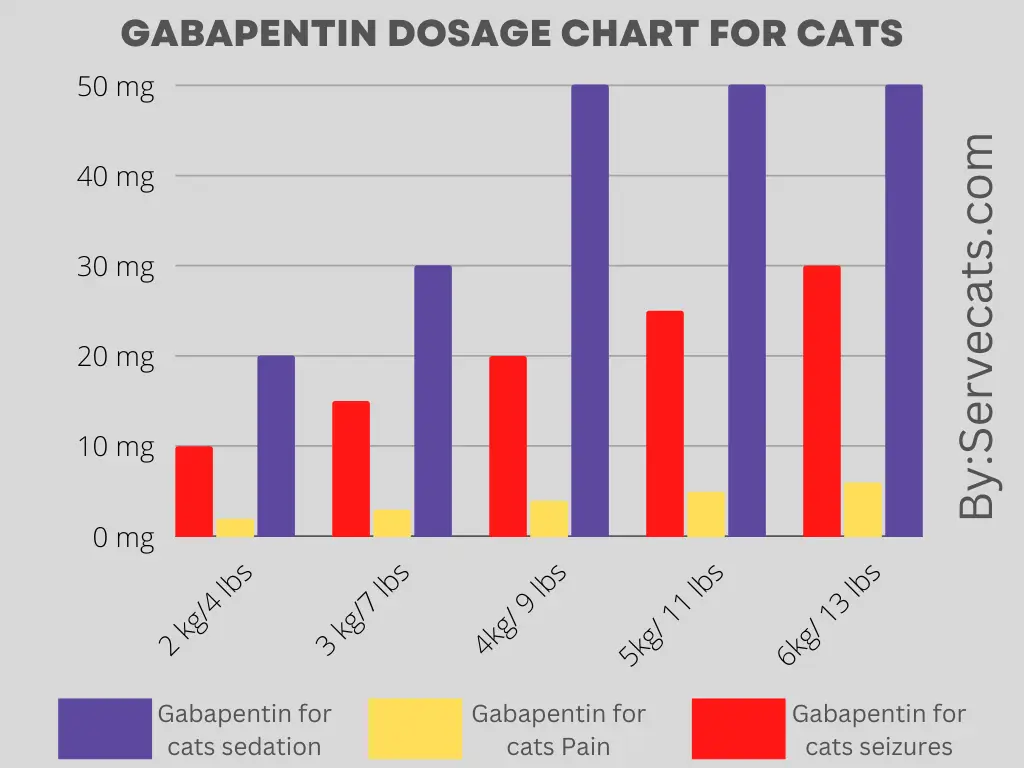
Document the dose reduction plan clearly for the person reducing their opioid or gabapentinoid medication, using the template available on East Sussex Formulary. If there is a planned reduction of gabapentinoid, this can be done as recommended on pages 2 and 3. Before starting: • Where possible, ensure any reduction is discussed and agreed with the patient. • Agree the speed of dose reduction with the patient. • Typically, one change per week is recommended. Some patients will need space to •A suggested reduction regime (full regime available in the full guide) for analgesic use would be: •Gabapentin –reduce at maximum daily rate of 300mg every week •Pregabalin - reduce at maximum daily rate of 50-100mg every week •In high risk patients, temporarily halt reduction, in preference to re-escalating the dose when required A trial reduction of gabapentinoid should be considered every 6-12 months, when prescribed for chronic pain. The dose should be reduced gradually to minimise withdrawal effects and check if there is any change in your pain. Please follow your reduction plan. You may need a prescription for different strengths of medication. Discuss with the patient that reduction can be paused, but not reversed. Total daily opioid dose should be reduced gradually when a person has been prescribed a strong opioid for longer than two weeks. PK !T ¼Ù© [Content_Types].xml ¢ ( Ä–ËnÂ0 E÷•ú ‘· 1°¨ªŠÀ¢ e‹Tú &ž€Ûø!{xý}' ¢ ‚ Q7‘’™{ï M"g0Zë mSÃi³L¥Pé 7çm !Ðfu W -”Ùó å0 = OÊëƒTÖ 79„ë ”¾Íñ€H‚6vÎ +˜~´Fñ˼ $³ Å6¶QY7B€‘-1ì æ $øÞõ Jã³öÐJ~i|æüý ž¿ü3çÏ(r"¦9´A°³n„@:t¡¼^þ&lmNERçØ[ è ÷ { ~ ê ìÀ£:ý¥U‰d}ñ|P Í dM6ßþÒ ÿÿ PK GMMMG Gabapentinoids - Prescribing for pain - Resource pack v. 1.1 4 Appendix 7 – Summary of GMMMG and NICE guidance for self-management and use of Following concerns about abuse, gabapentin has been reclassified as a Class C controlled substance and is now a Schedule 3 drug, but is exempt from safe custody requirements. Healthcare professionals should evaluate patients carefully for a history of drug abuse before prescribing gabapentin, and observe patients for signs of abuse and dependence. • Gabapentin could be reduced by 300mg per week • Pregabalin could be reduced by 75mg per week Please follow your reduction plan. Gabapentin and pregabalin come in different strengths. You may require different strengths to allow you to follow the reduction plan. Do not try to reduce at stressful times or when your pain is flared up. Gabapentinoids have been reclassified as Schedule 3 CDs under the Misuse of Drugs Regulations 2001 and Class C controlled substances under the Misuse of Drugs Act 1971 from 1st April 2019. Dose reduction should be gradual, for example stepping down every 10 days but no faster than once a week, unless advised and supervised by a health care professional. Please see table overleaf for your individual gabapentinoid reduction plan. A trial of dose reduction/cessation should be undertaken after two months of relative improvement in pain following stabilisation on treatment. A suggested reduction regimen would be: Gabapentin – reduce at maximum daily rate of 300mg every week . Pregabalin – reduce at maximum daily rate of 50-100mg every week Reduction in pain by 50% is a commonly used endpoint in clinical trials. Screening tools can also be useful to aid diagnosis: the Neuropathic Pain Scale Pregabalin or Gabapentin (note 1) Switch to the one which was not used first (gabapentin or pregabalin) if not tolerated Dose Titration Notes Pregabalin Initially 150mg in 2-3 divided doses. Max. 600mg daily Aim for twice a day dosing with pregabalin (benefit cost and compliance). maximum of 600mg/day after (150mg bd - £12.12) see appendix 1 Prepare medication reduction schedule*: Recommend 10% reduction every one to two weeks tailored to needs of patient. Start with reducing short-acting medicines followed by long-acting medicine Start from the most relevant point of the schedule depending on the patient’s current dose. Oxford University Hospital templates for opioid reduction** • If a patient develops acute pancreatitis, gabapentin discontinuation should be considered • History of substance abuse, psychotic illness. • Diabetes mellitus. Drug interactions • Gabapentin with opioids or TCAs: CNS depression. • Gabapentin with TCAs or duloxetine: increased risk of hyponatraemia Time to response: 2 weeks. Time to Gabapentin should be taken at least 1 hour before, or 3 hours after, sevelamer if the reduction in gabapentin levels is clinically significant. Morphine — interaction of gabapentin with morphine sulphate increases risk of respiratory depression. Why have I been prescribed Gabapentin? • Gabapentin is used to treat some types of persistent pain. • It is especially good for nerve pain, such as burning, shooting or stabbing pain. • Gabapentin belongs to a group of medicines called anticonvulsants which are also used to treat epilepsy. Gabapentinoid Prescribing: Primary Care Update. Background. Prescribing teams in NHSGGC have been reviewing patients prescribed gabapentinoids (gabapentin and pregabalin) over the past year with an aim of reducing prescribing where it is safe and appropriate to do so Gabapentin: 1200mg-3600mg/day in three divided doses for 3-8 weeks. - An adequate trial should include at least 2 weeks at the maximum tolerated dose before deciding gabapentin is ineffective. - Consider switching to pregabalin: 150mg to 600mg/day for 4 weeks if intolerable side-effects occur. - Advice on switching can be found here. 3rd line:
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |