Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 | 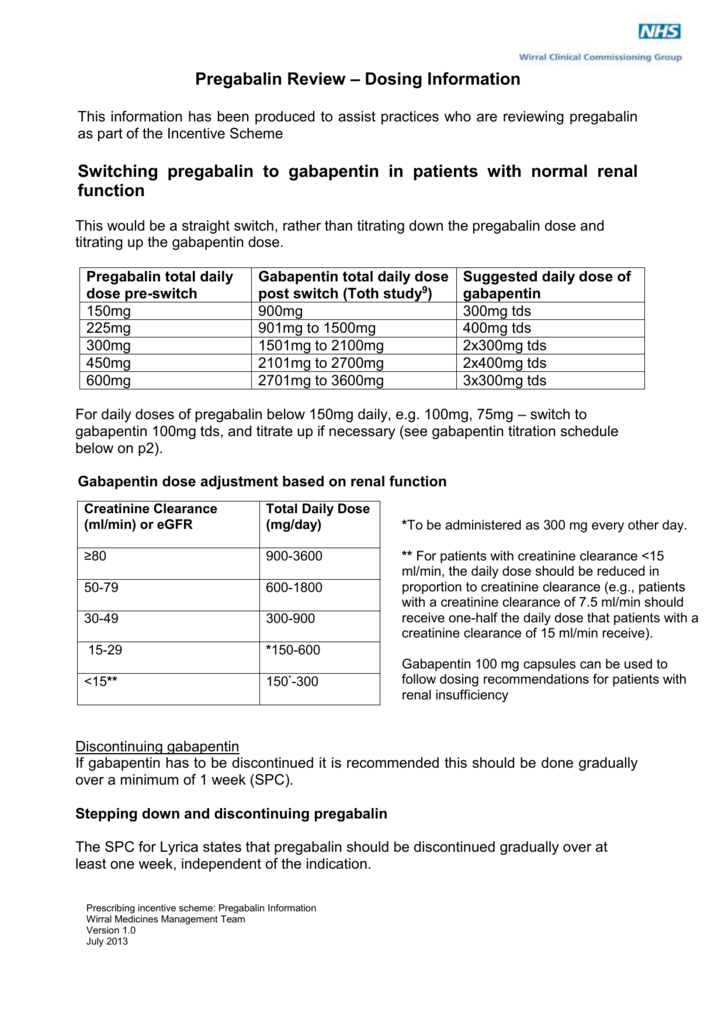 |
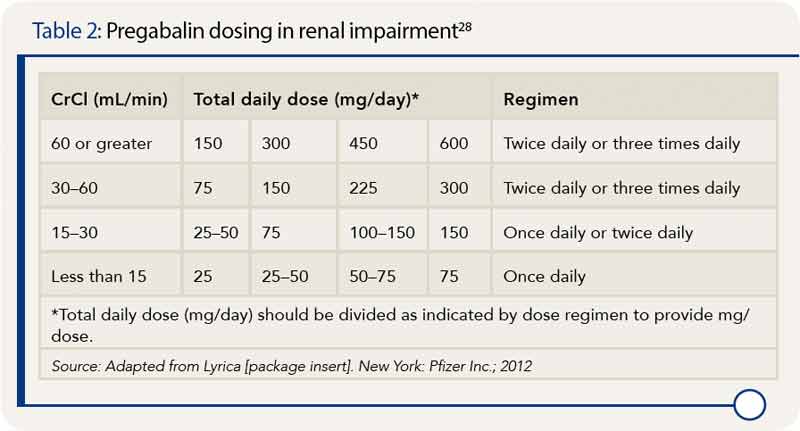
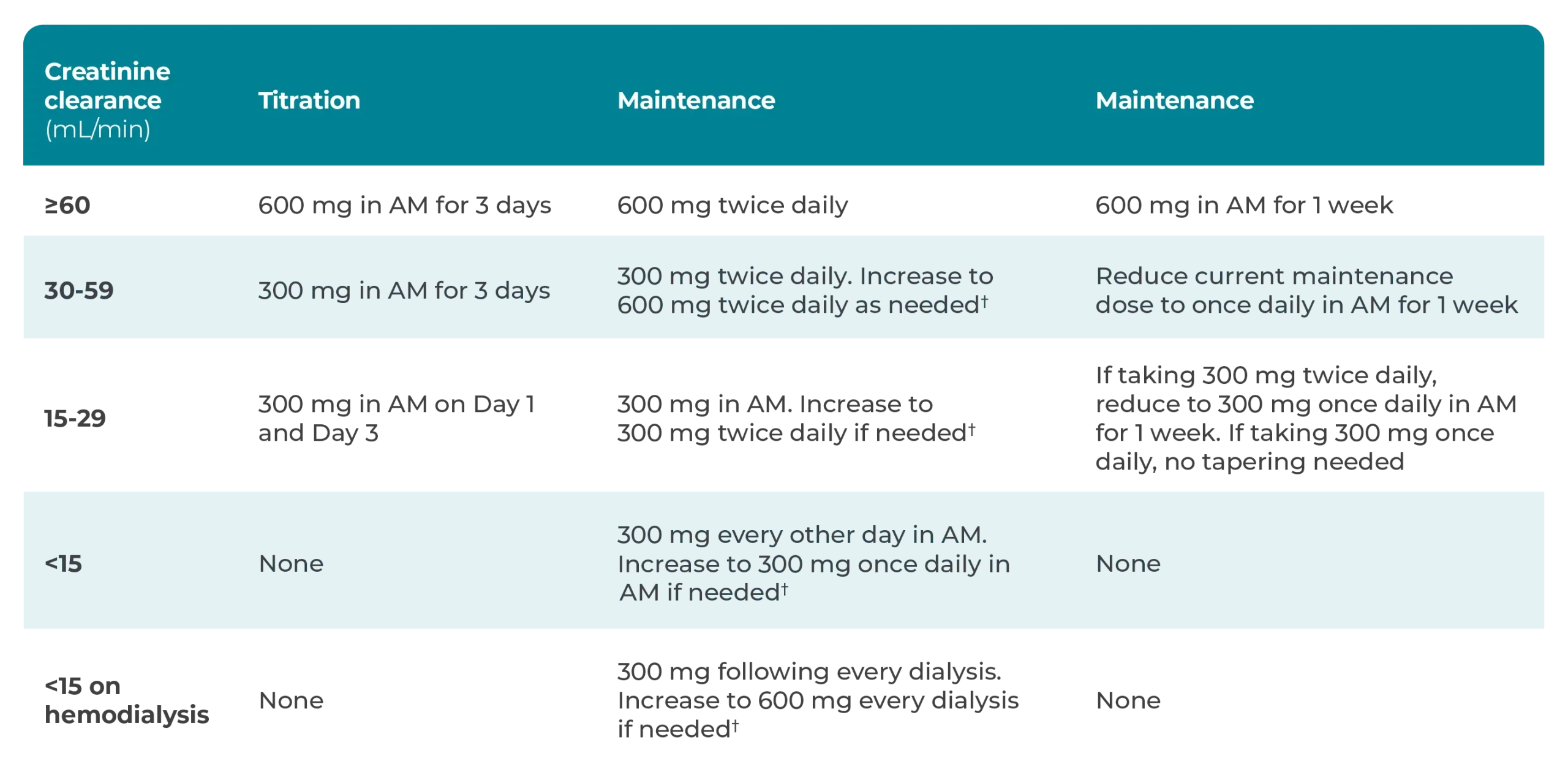
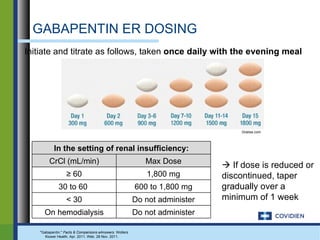
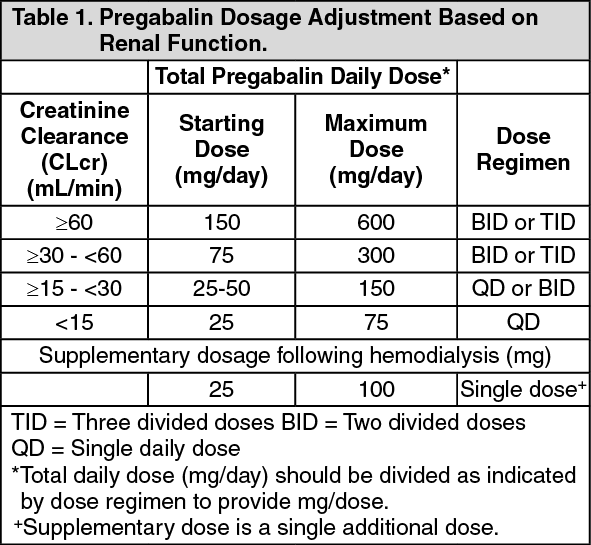
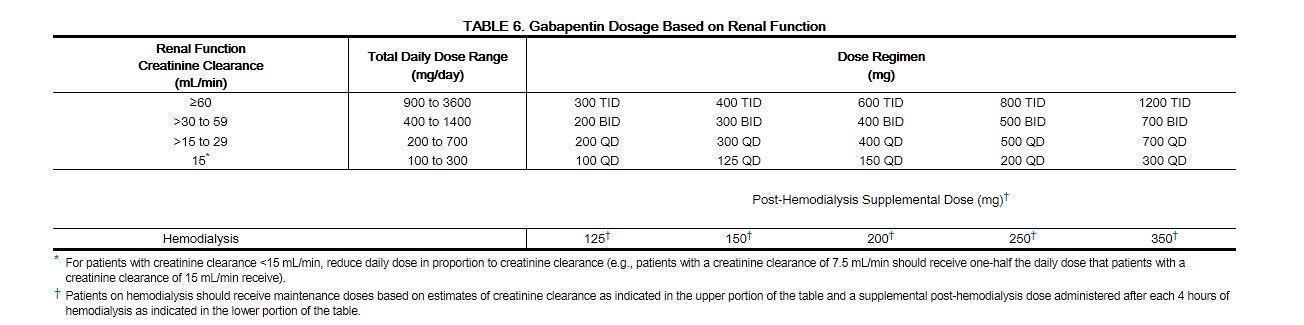
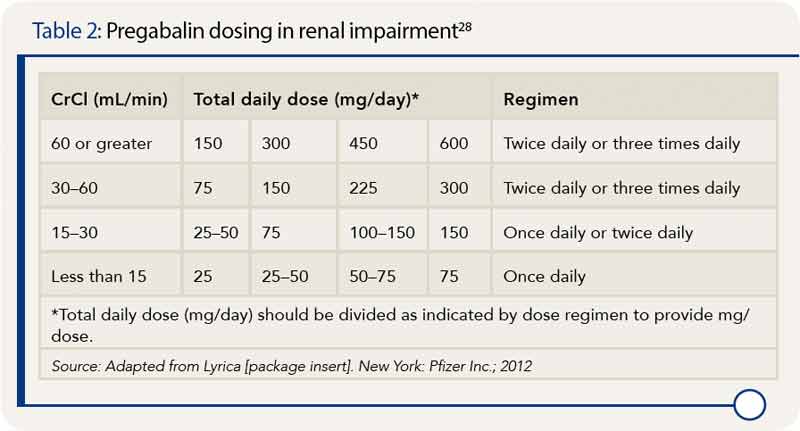
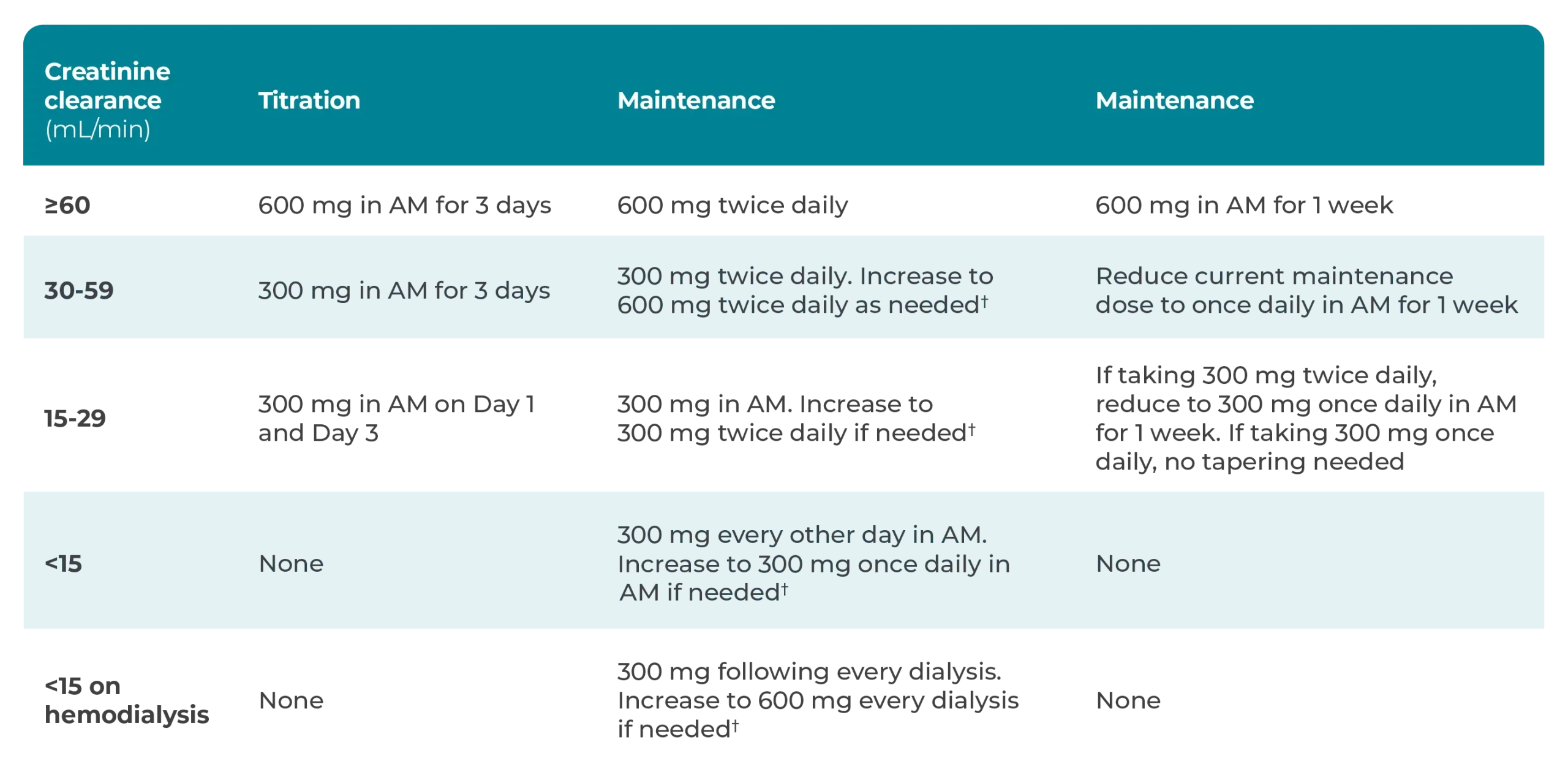
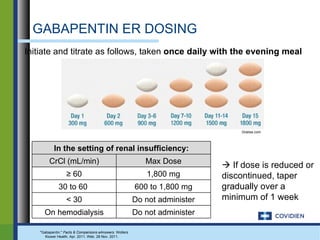
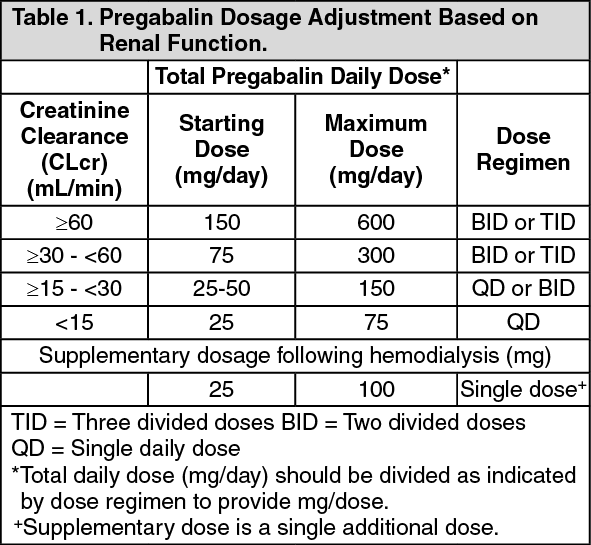
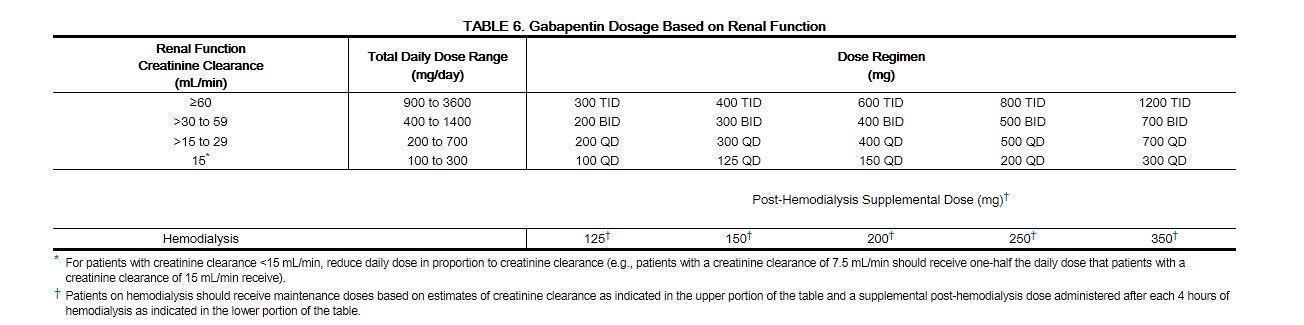
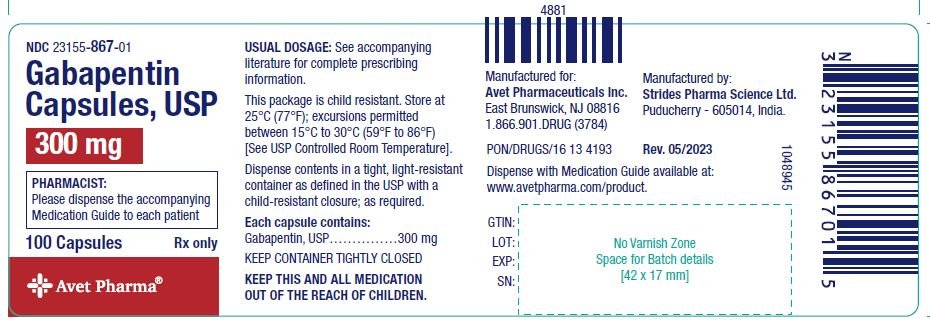
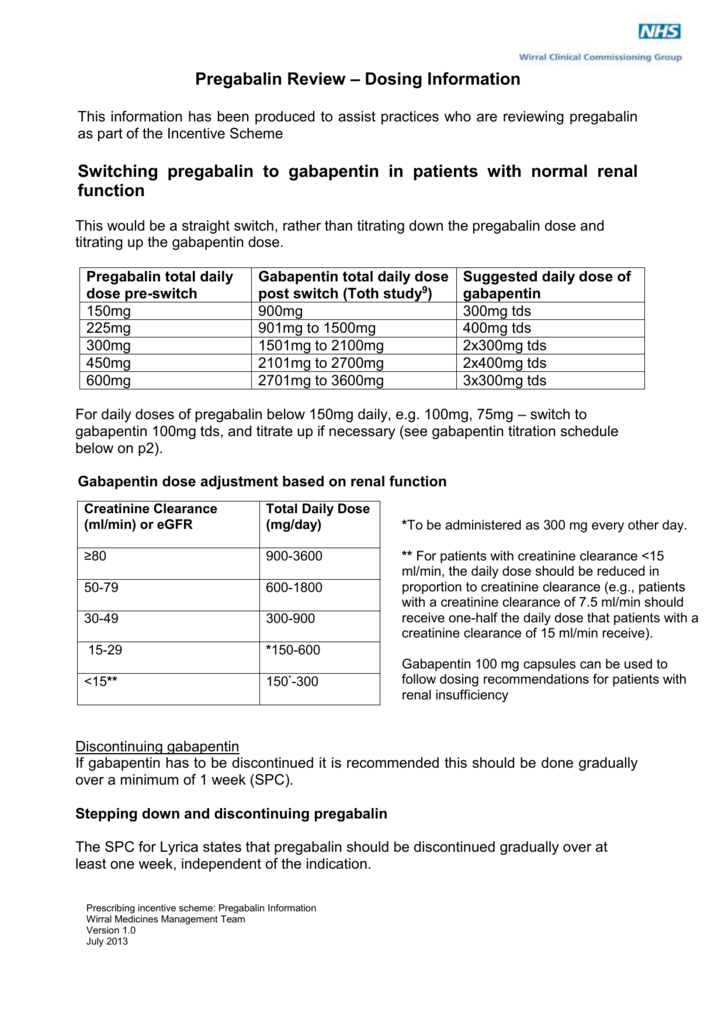
4. Renal Dosing Recommendations. Mild Kidney Problems (CrCl 60-90 mL/min): Dose Adjustment: 900 - 3600 mg/day TID. How Often to Take: 3 times a day. Notes: Monitor for dizziness or double vision. Moderate Kidney Problems (CrCl 30-59 mL/min): Dose Adjustment: 400-1400 mg/day BID; How Often to Take: Twice a Day; Notes: Your doctor will decide the Notwithstanding, most reports of toxicities were associated with concentrations higher than 15 mg/L for gabapentin and concentrations higher than 13 mg/L for pregabalin, whereas individuals with normal renal function on maximum recommended dosing yielded concentrations of ~5–8 mg/L for gabapentin and 2.8–8.2 mg/L for pregabalin. 22–25 The The recommended dose of gabapentin in dialysis patients is 100 to 300 mg/per day, but on dialysis day an additional dose is given after the session, due to drug clear-ance through the dialysis membrane. We prescribed 300 mg/day (in a capsule), the minimum available dose of gabapentin in Greece. However, on dialysis day we gave Pain in Dialysis Patients and from work of Dr. S. Davison. RECOMMENDED Acetaminophen Hydromorphone Fentanyl Methadone Gabapentin Has saturable absorption. Titrate slowly; doses up to 300 mg per day are generally considered safe in dialysis patients. Pregabalin Has similar efficacy and side effects as gabapentin. May be useful in patients Dosages of drugs cleared renally should be adjusted according to creatinine clearance or glomerular filtration rate and should be calculated using online or electronic calculators. Recommended Renal Dosing; CrCl>60 mL/min: 300-1200mg PO TID CrCl 30-60 mL/min: 200-700mg q12hr CrCl 15-29 mL/min: 200-700mg qDay CrCl<15 mL/min: 100-300mg qDay HD: 125-350mg posthemodialysis after each 4h dialysis interval. Hepatic Dosing Adult: no modifications; Pediatric: no modifications; Contraindications. Allergy to class/drug; Adverse Reactions Serious It is recommended that patients with end-stage renal disease maintained on hemodialysis receive an initial 300-mg to 400-mg gabapentin loading dose. Plasma gabapentin concentrations can be maintained by giving 200 to 300 mg of gabapentin after every 4 hours of hemodialysis. Dosage Adjustment in Patients with Renal Impairment . Dosage adjustment in patients 12 years of age and older with renal impairment or undergoing hemodialysis is recommended, as follows (see dosing recommendations above for effective doses in each indication): Reference ID: 4584064 . This label may not be the latest approved by FDA. A few small studies have suggested that pain is as common among peritoneal dialysis patients and stage 5 CKD patients who are not on dialysis as among chronic hemodialysis patients . To continue reading this article, you must sign in with your personal, hospital, or group practice subscription. Dosage adjustment in patients 12 years of age and older with renal impairment or undergoing hemodialysis is recommended, as follows (see dosing recommendations above for effective doses in each indication): TABLE 1. Gabapentin Dosage Based on Renal Function Renal Function Creatinine Clearance (mL/min) Total Daily Dose Range (mg/day) Dose normal renal function on maximum recommended dosing yielded concentrations of 5–8 mg/L for gabapentin and ~ 2.8–8.2 mg/L for pregabalin. 22–25 The elimination half-lives of gabapentin and pregabalin are prolonged with renal impairment leading up to accumulation with repeated dosing. The half-life of gabapentin immediate-release The recommended dose of gabapentin in dialysis patients is 100 to 300 mg/per day, but on dialysis day an additional dose is given after the session, due to drug clearance through the dialysis membrane. We prescribed 300 mg/day (in a capsule), the minimum available dose of gabapentin in Greece. Gabapentin dosing guidelines for adult with renal impairment are summarized in Table 3. Dosing guidelines for gabapentin immediate-release are also applicable for adolescents 12 years of age and older with renal impairment. In patients with normal renal function, the maximum dose of gabapentin is 3600mg daily in divided doses. However, gabapentin is renally cleared and so the dose needs to be adjusted according to the GFR. For patients on dialysis, the recommended dose is 100-300mg post dialysis on dialysis days only. Give supplemental dose of 125-350mg after each dialysis. Dosage given should be proportional to maintenance dose. Patients receiving at least 300mg/day can be given the higher supplemental dose of 350mg after each dialysis. Other patients should receive a dosage at the lower end of this range. [See above for updated info from the package insert] Detailed Gabapentin dosage information for adults and children. Includes dosages for Restless Legs Syndrome, Epilepsy and Postherpetic Neuralgia; plus renal, liver and dialysis adjustments. The half-life of gabapentin immediate-release formulation is 5–7 hours in patients with normal renal function and is prolonged up to 52 hours in patients with CrCl<30 mL/min. 26 The half-life of pregabalin is 16.7 hours in patients with CrCl 30–59 mL/min, 25 hours in patients with CrCl 15–29 mL/min, and 48.7 hours in patients with CrCl<15 Renal clearance of gabapentin may vary in different dialysis patients depending on residual renal function and a lower starting dose is recommended for patients who are anuric. From the adverse events that were reported, they often subsided over 5–10 days [ 17 , 19 ]. Maximum dose: 75 mg/day. Dose to be given post-HD on HD days. No data to support use of pregabalin in gabapentin resistant or intolerant patient. THC:CBD (Sativex®): 1 spray under tongue or toward inside of cheeks daily to bid. May increase by 1 spray/day q2-4 days. Maximum dose: 12 sprays/day. Limited data in renal failure patients. Loading dose of 300–400 mg in patients who have never received gabapentin. Maintenance dose of 100–300 mg after each HD : session and increase according to tolerability.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |