Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 | |
 | |
 |  |
 |  |
 |  |
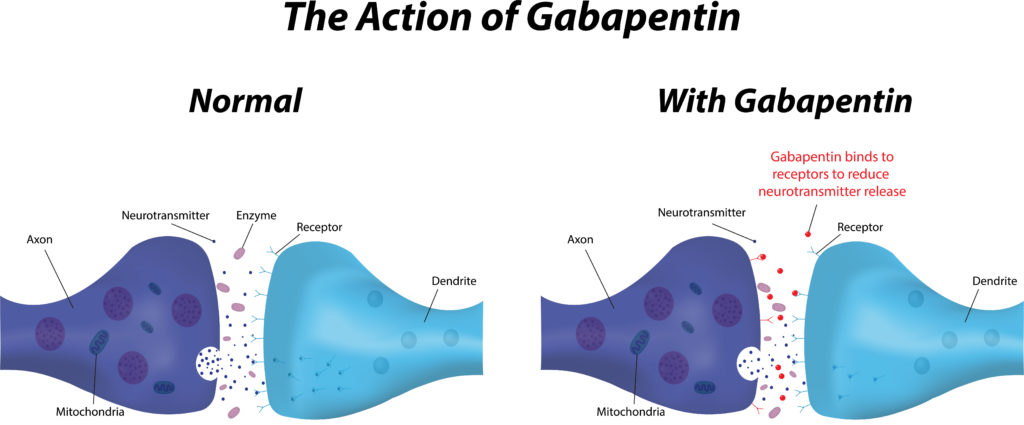
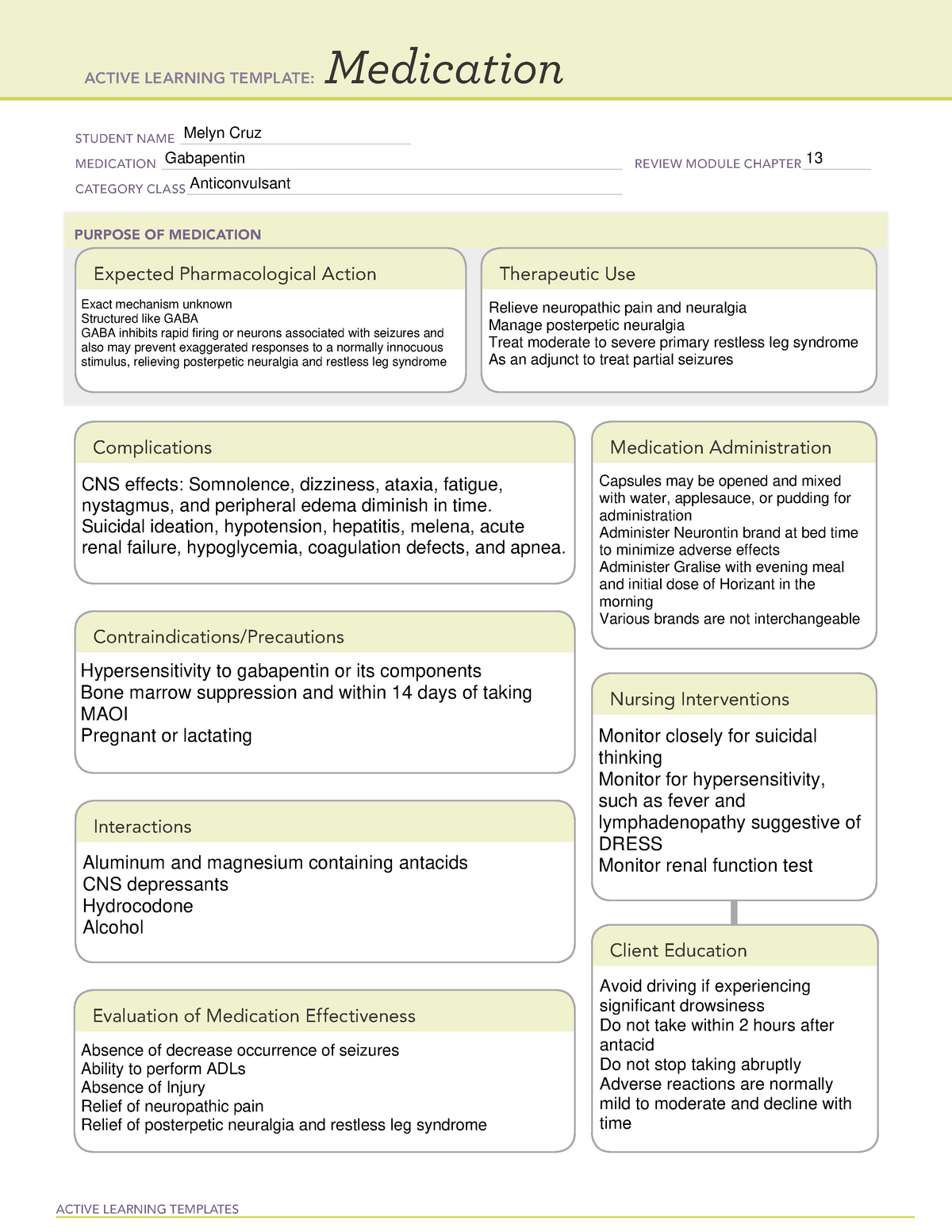
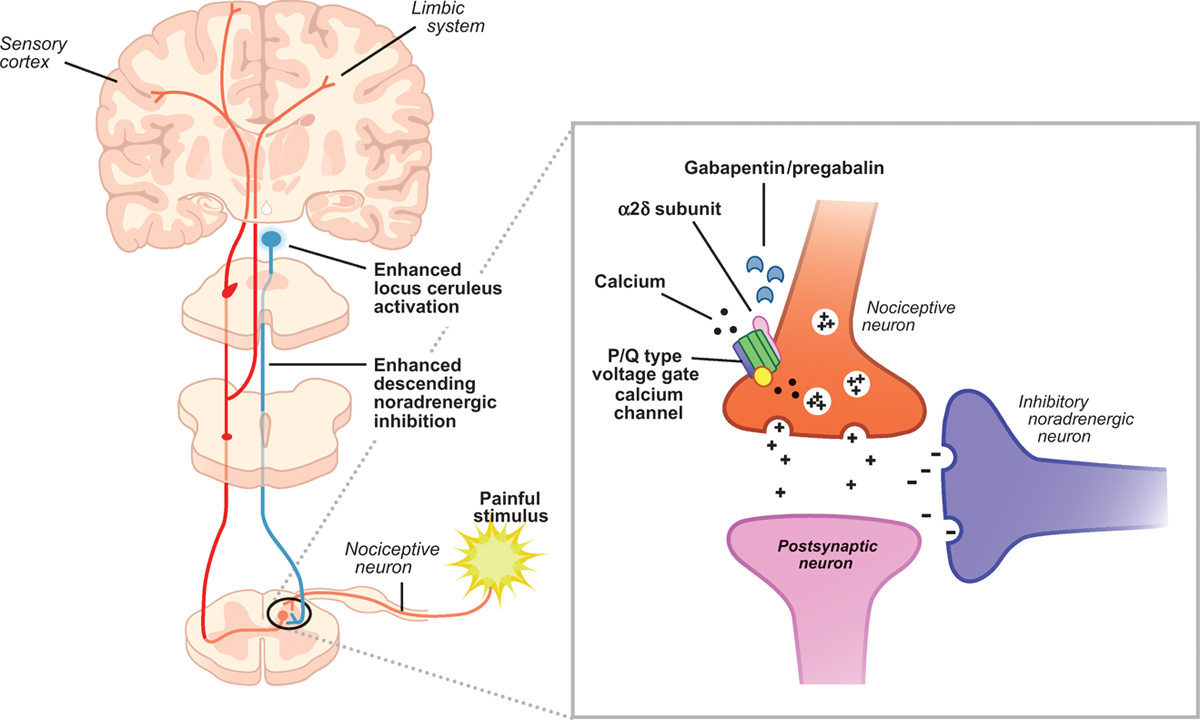
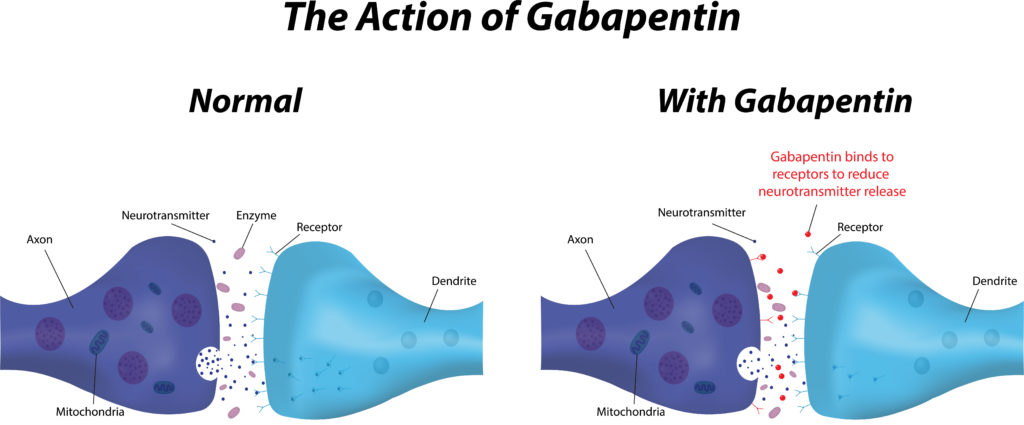
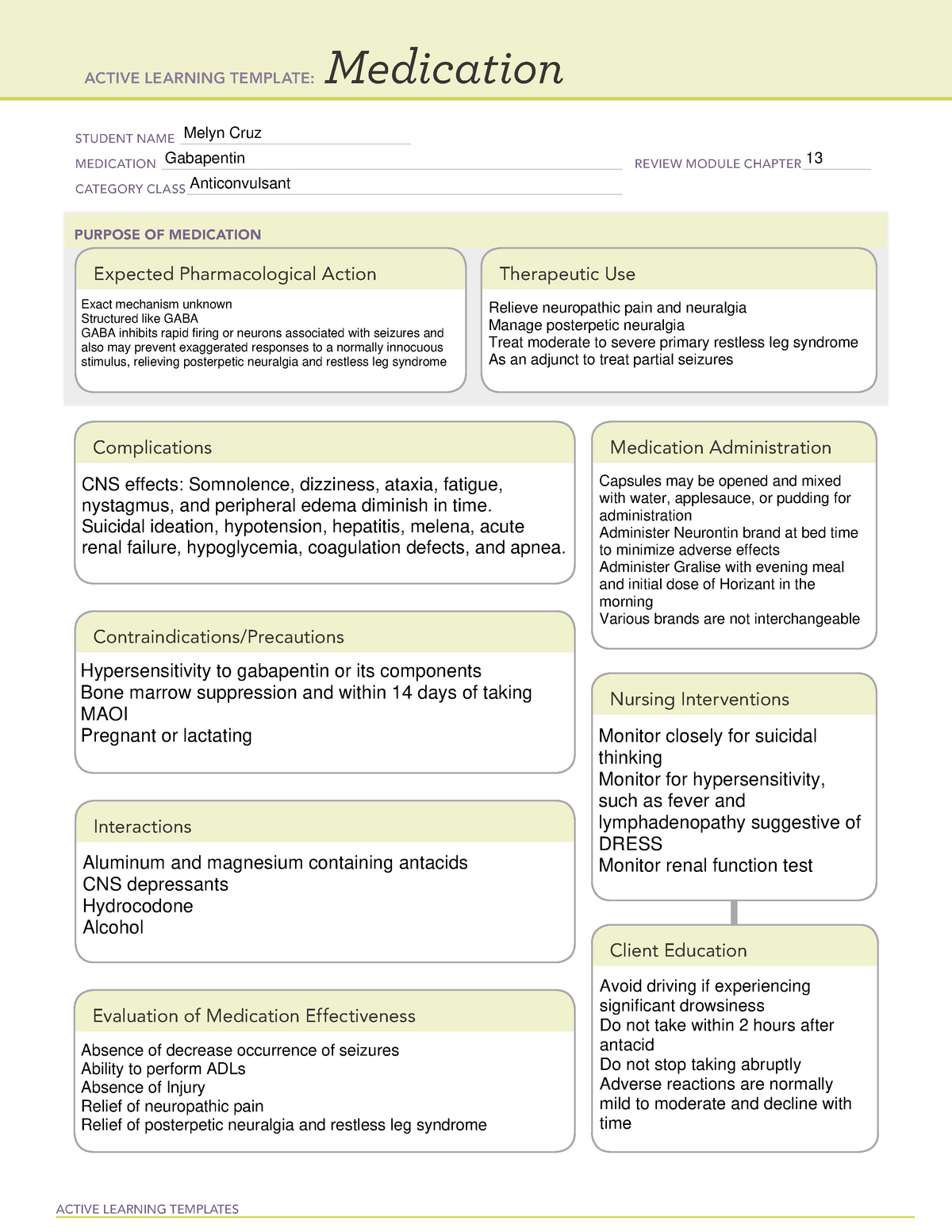
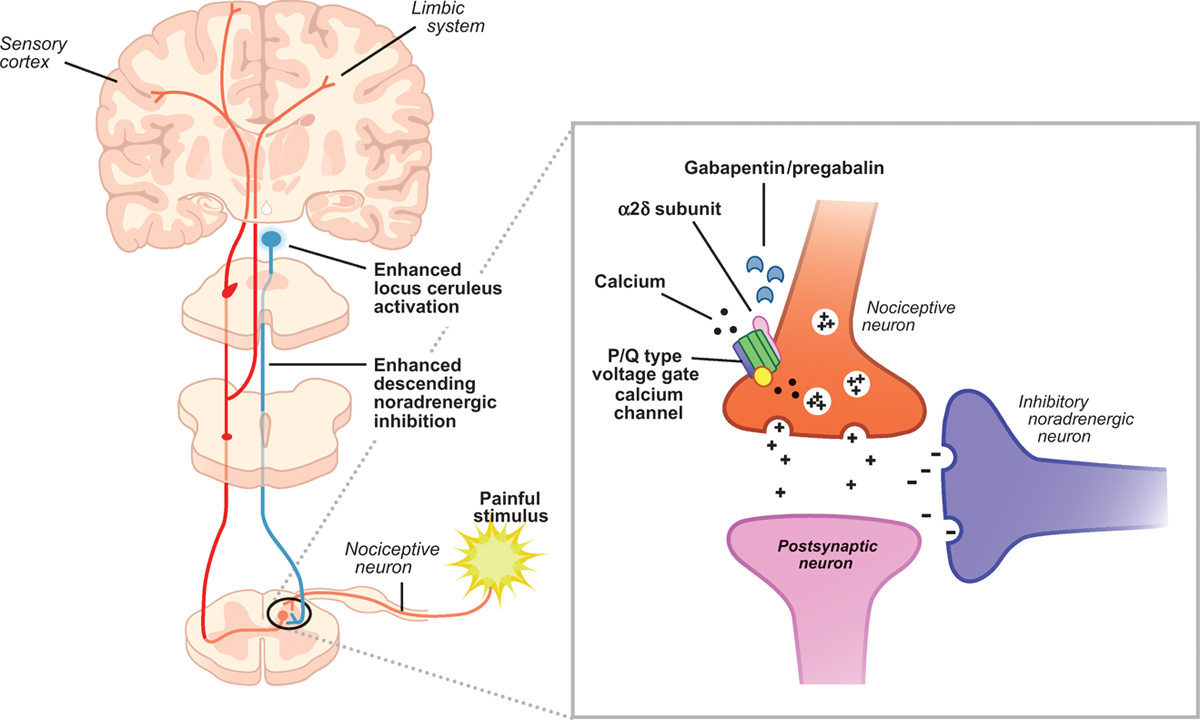
Gamma-aminobutyric acid (GABA) and glutamate (GLU) play crucial roles in the control of neuropathic pain through their actions within the central nervous system (CNS). These neurotransmitters separately activate two distinct classes of receptors: ionotropic and metabotropic. Mechanism of action. The precise mechanism through which gabapentin exerts its therapeutic effects is unclear. 16,17 The primary mode of action appears to be at the auxillary α2δ-1 subunit of voltage-gated calcium channels (though a low affinity for the α2δ-2 subunit has also been reported). 10,8,14 The major function of these subunits is The mechanisms of the anti-allodynic effects of gabapentin proposed include: CNS effects (potentially at spinal cord or brain level) due to either enhanced inhibitory input of GABA-mediated pathways (and thus reducing excitatory input levels); antagonism of NMDA receptors; and antagonism of calcium channels in the CNS and inhibition of Gabapentin is a potent activator of voltage-gated potassium channels KCNQ3 and KCNQ5, even at low nanomolar concentrations. However, this activation is unlikely to be the dominant mechanism of gabapentin's therapeutic effects. [90] Gabapentin is a structurally related to GABA that binds to voltage-gated calcium channels. It is used for various conditions such as epilepsy, neuropathic pain, restless legs syndrome, and postoperative pain. This activity outlines the indications, mechanisms of action, administration, significant adverse effects, contraindications, monitoring, and characteristics of gabapentin toxicity. This activity also provides clinicians with the necessary skills and tools to treat various types of muscular, neurological, and psychiatric medical conditions Gabapentin and pregabalin are structurally related compounds with recognized efficacy in the treatment of both epilepsy and neuropathic pain. The pharmacological mechanisms by which these agents exert their clinical effects have, until recently, remained unclear. The interaction of gabapentin and pr Busch et al. reported that antacids reduce the bioavailability of gabapentin by ≈ 20% when given concomitantly with, or up to 2 h post, gabapentin administration . Mechanism of action. Gabapentin has no direct GABAergic action and does not block GABA uptake or metabolism. Gabapentin Mechanism of action. Gabapentin does not act directly on GABA receptors in spite of their close structural resemblance to GABA. They may, however, modify the synaptic or nonsynaptic release of GABA. An increase in brain GABA concentration is observed in patients receiving gabapentin. Although the exact mechanism of action with the GABA receptors is unknown, researchers know that gabapentin freely passes the blood-brain barrier and acts on neurotransmitters. Gabapentin has a cyclohexyl group to the structure of the neurotransmitter GABA as a chemical structure. In vitro, gabapentin modulates the action of the GABA synthetic enzyme, glutamic acid decarboxylase (GAD) and the glutamate synthesizing enzyme, branched-chain amino acid transaminase. Results with human and rat brain NMR spectroscopy indicate that gabapentin increases GABA synthesis. Several mechanisms of gabapentin have been proposed after neuropathy including an inhibition of NMDA receptors, inhibition of sodium currents and reducing β4a subunit mediated VGCC trafficking (Hara and Sata 2007; Mich and Horne 2008; Yang et al. 2009). Mechanism of Action Gabapentin is designed as GABA analog (similar to pregabalin ), which means it binds to the α2δ (alpha-2-delta) subunit of presynaptic voltage-sensitive Ca2+ channels (VSCCs), and block the release of excitatory neurotransmitters such as glutamate. Mechanism of action By inhibiting the voltage-gated calcium channels in the CNS, gabapentin reduces the release of excitatory neurotransmitters (mostly noradrenaline, dopamine and serotonin), and therefore decreases epileptogenesis. As with many other agents, GBP was licensed for the treatment of epilepsy with little or no understanding of its mechanism of action. Continued research and the parallel development of PGB have contributed to a contemporary pharmacological view of GBP (and PGB) as drugs with multiple modest cellular effects at therapeutic concentrations, but with a single predominant mechanism of action that Pregabalin and gabapentin share a similar mechanism of action, inhibiting calcium influx and subsequent release of excitatory neurotransmitters; however, the compounds differ in their pharmacokinetic and pharmacodynamic characteristics. Gabapentin is absorbed slowly after oral administration, with m Gabapentin is an anti-epileptic agent but now it is also recommended as first line agent in neuropathic pain, particularly in diabetic neuropathy and post herpetic neuralgia. α2δ-1, an auxillary subunit of voltage gated calcium channels, has been documented as its main target and its specific binding to this subunit is described to produce different actions responsible for pain attenuation Mechanisms of action. Gabapentin and pregabalin do not bind to GABA receptors despite their structural similarity but have a high affinity for the α2δ-1 subunit of voltage-gated calcium channels (VGCCs). 19 VGCCs are composed of multiple subunits: α 1, β, γ and α 2 δ. Mechanism of Action Although gabapentin is a structural analog of the neurotransmitter gamma-aminobutyric acid (GABA), it appears not to interact with GABA receptors. Its mechanism of action is not entirely clear but is likely related to inhibition of calcium and, possibly, sodium channels. 1 Mechanism of action of gabapentinoids Site of action The actions of gabapentinoids are mainly at an intracellular site and require active uptake.21 They were originallydesigned as g aminobutyric acid (GABA) analogues but do not have any effects on GABA receptors. Gabapentin binds to a 2d receptors with greater affinity to the a 2d-1 subtype.22
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 | |
 | |
 |  |
 |  |
 |  |