Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
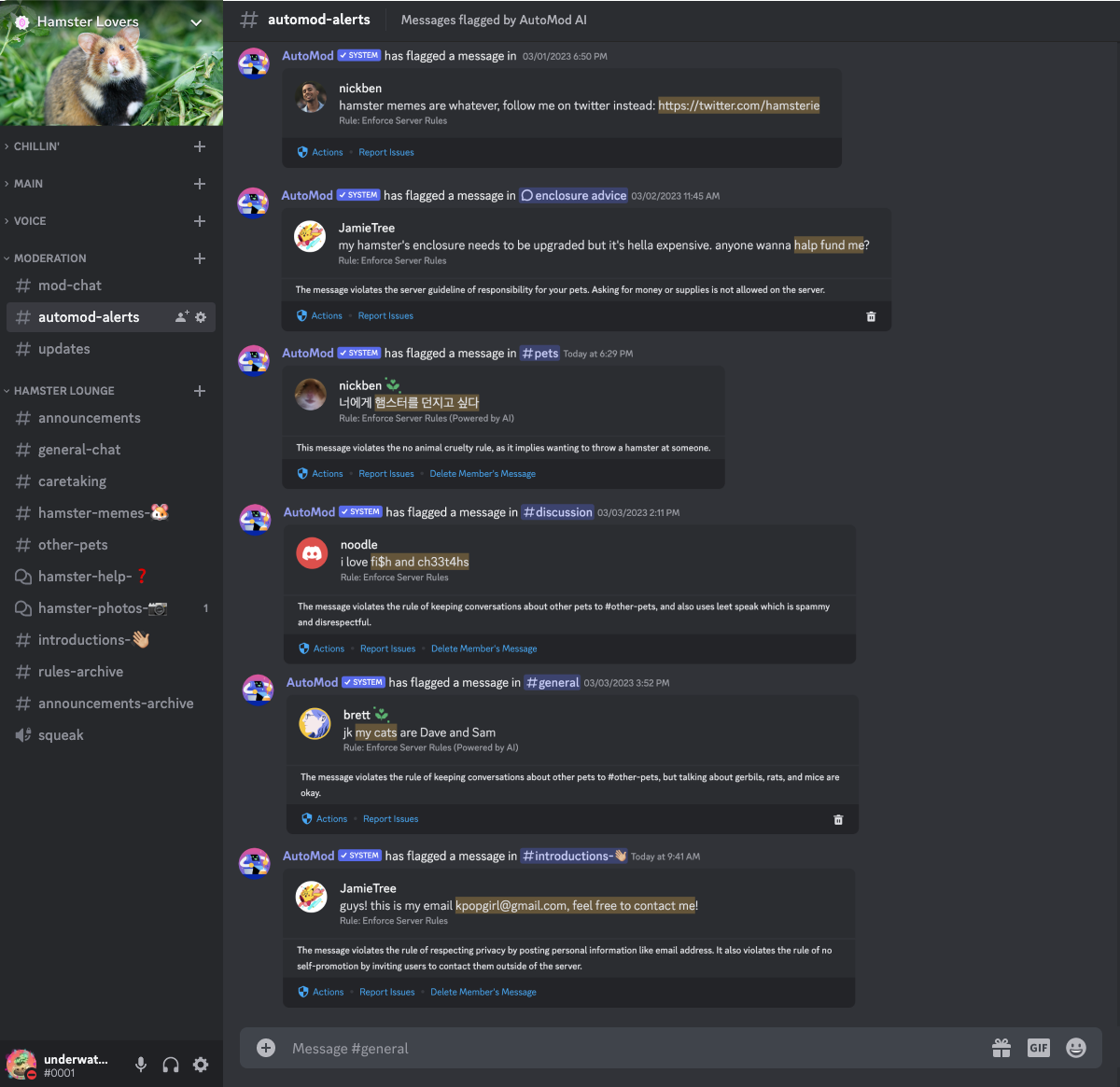
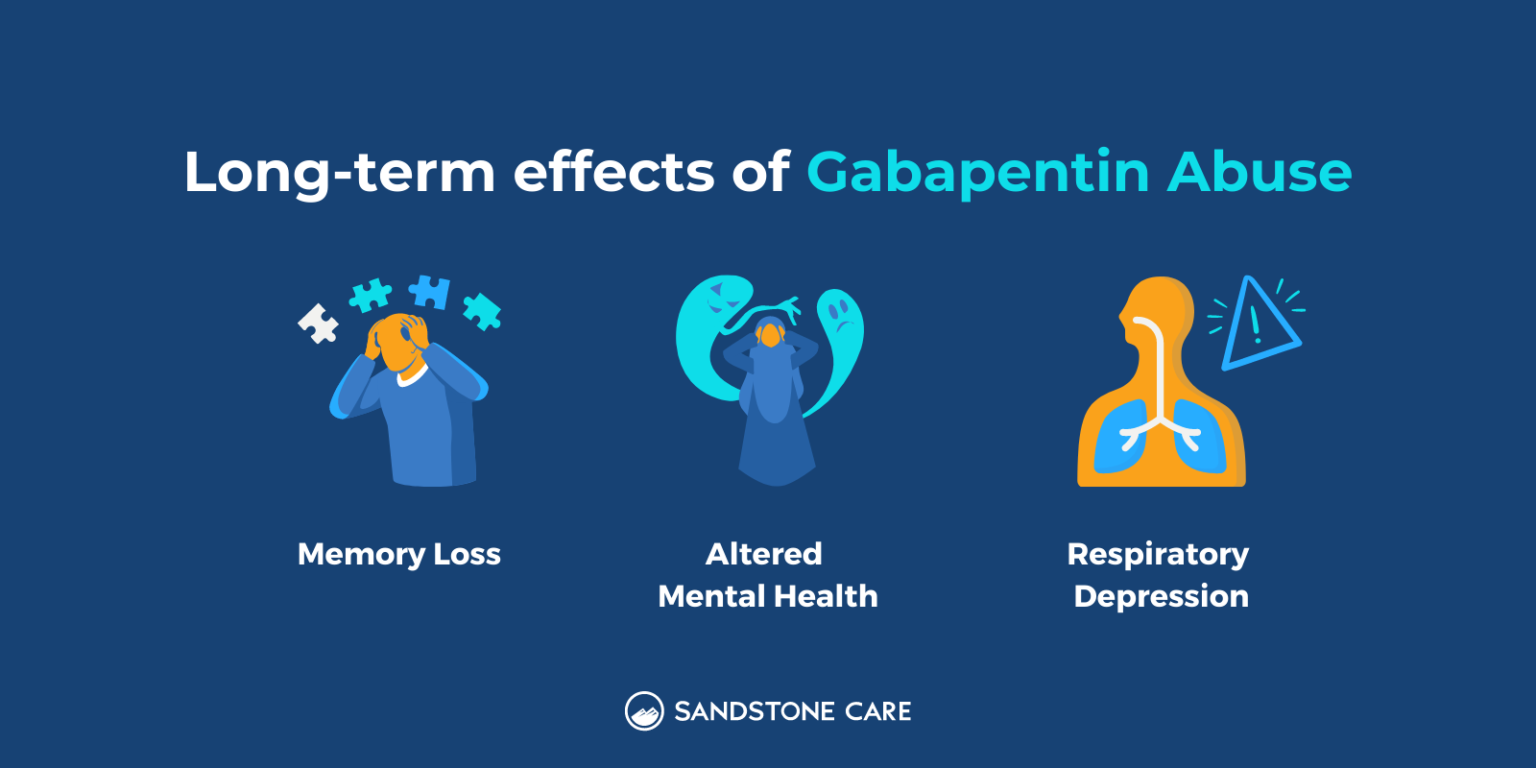
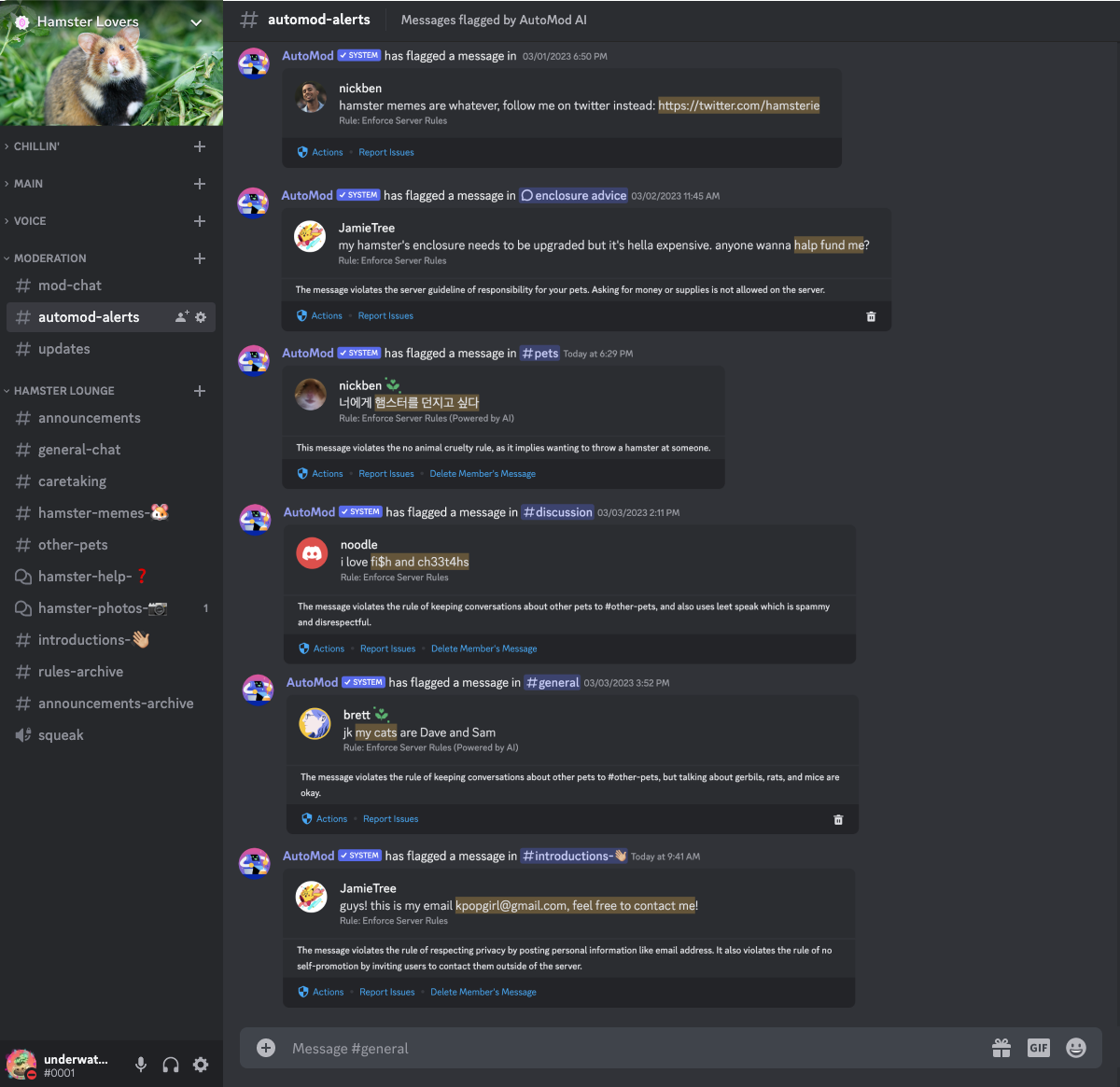
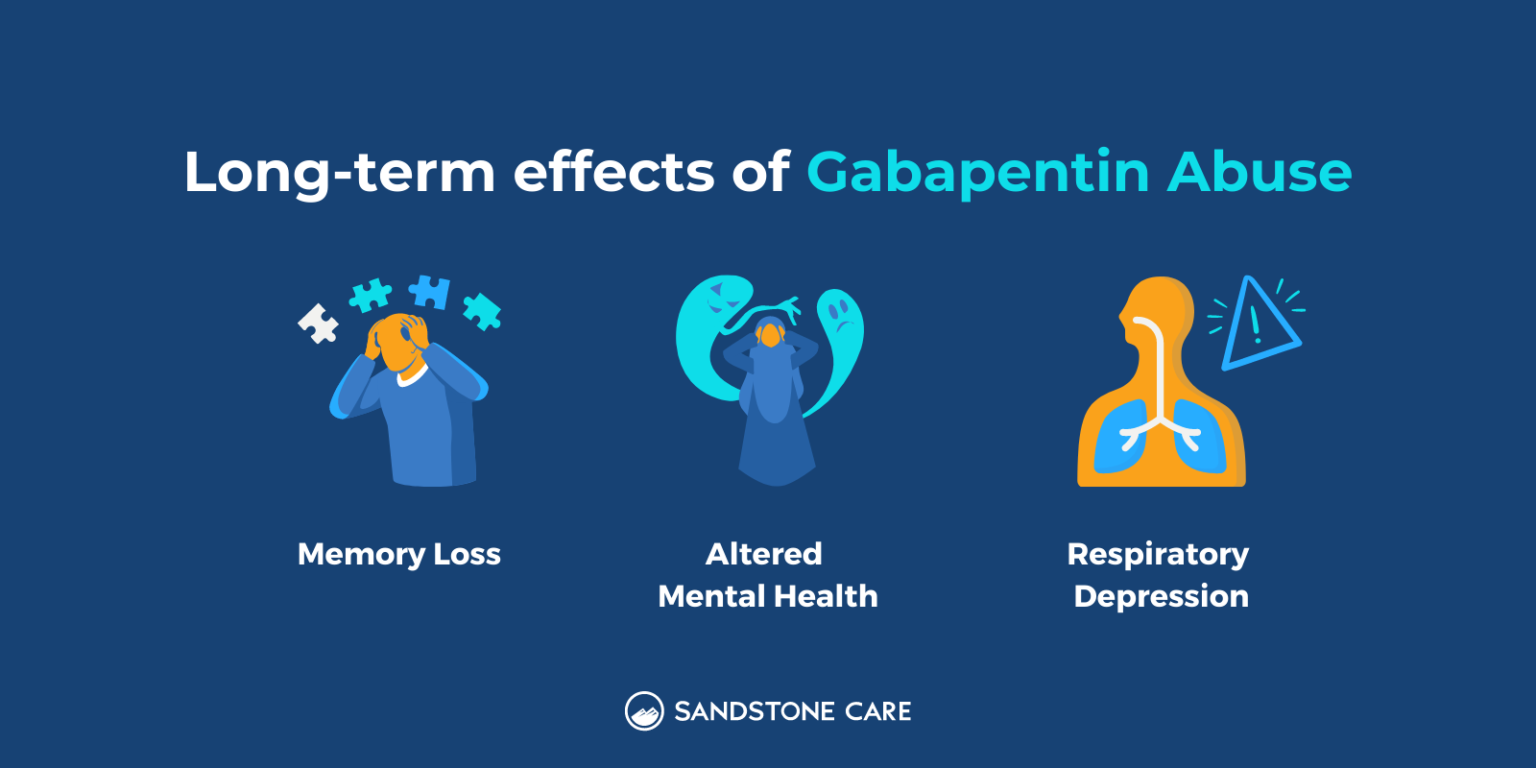
Practitioners should prescribe pregabalin and gabapentin appropriately to minimise the risks of misuse and dependence, and should be able to identify and manage problems of misuse if they The use of gabapentin and pregabalin by the opioid abusing population either together or when opioids are unavailable reinforces the behaviour patterns of this high risk population. This review summarizes current evidence on the abuse and misuse of the gabapentinoids pregabalin and gabapentin. Pharmacovigilance studies, register-based studies, surveys, clinical toxicology studies, and forensic toxicology studies were identified and scrutinized with the goal to define the problem, identify risk factors, and discuss possible methods to reduce the potential for abuse and Available evidence also suggests that abuse and misuse are more frequent in users of pregabalin compared with users of gabapentin. Health professionals and prescribers should be aware of the risk for misuse of pregabalin and gabapentin, which eventually could lead to abuse, substance dependence, and intoxications. Gabapentin is one of the recommended mainstays of evidence-based treatment.3. Unfortunately, our clinical experience suggests that gabapentin is now prevalent as a drug of abuse. The drug’s effects vary with the user, dosage, past experience, psychiatric history, and expectations. Dependence on pregabalin is especially dangerous for those with a prior history of drug abuse or addiction. How can you come off it, and is withdrawal an issue? Some people find it hard to stop Studies found that gabapentinoids are abused and misused and that individuals with a history of psychiatric disorders or substance use disorder seem to be at high risk. Moreover, some evidence supports the notion that patients with opioid use disorders may be at an increased risk of abusing gabapentinoids. Background A 2017 systematic review (SR) identified 59 studies examining gabapentinoid (pregabalin and gabapentin) misuse/abuse. Evidence of gabapentinoid misuse/abuse has since grown substantially. Objective Update previous SR and describe new insights regarding gabapentinoid abuse. Methods A SR of PubMed was conducted to identify studies published from 7/29/2016–8/31/2020. Four searches In this study we examined deaths following gabapentinoid use in England reported to the National Programme on Substance Abuse Deaths. A total of 3051 deaths were reported (gabapentin: 913 cases; pregabalin: 2322 cases [both detected in 184 cases]). Pregabalin was launched in the UK in 2004 while gabapentin was first authorised in the UK in 1997. Both drugs were originally licensed for seizure dis orders but now have multiple licensed indications. In England during 2016, over 12 million prescription items were dis pensed for gabapentinoids as a group.1 The Advisory Council on the Misuse of Published studies of anonymised primary care data using the UK Clinical Practice Research Datalink (CPRD GOLD) reported a tripling in the rate of incident gabapentin prescribing between 2007 and 2017, 4 with 50% attributed to an unlicensed indication in 2017, more than three times higher than in 2005 4; and a three-fold increase in incident Evaluate patients carefully for a history of drug abuse before prescribing pregabalin and gabapentin and observe patients for development of signs of abuse and dependence. The product A recent police report indicates the increasing tendency to use gabapentin as a ‘cutting agent’ in street heroin (and to recover gabapentin on the street and in prisons), further adding to the abuse and danger potential. 5 Like opiates, gabapentin is fatal in overdose; unlike opiates, there is no antidote and the long half-life instils the The gabapentinoid group consists of gabapentin and pregabalin. Structurally similar to the inhibitory neurotransmitter GABA (gamma-aminobutyric acid), gabapentinoids bind to a subunit (protein α2-δ) of a voltage-dependent calcium channel in the central nervous system, decreasing the intracellular calcium influx induced by cell depolarization, and the release of exciting neurotransmitters. Of the 11 population-based studies and 23 case reports included here, nearly one-third report gabapentin misuse/abuse for recreational purposes and epidemiological studies from the US and UK estimate abuse rates between 40–65% just among individuals with a gabapentin prescription. The gabapentinoid drugs, gabapentin and pregabalin, are first-line treatments for neuropathic pain. The epidemics of chronic pain and opioid misuse have given rise to the widespread use of non-opioid drugs such as the gabapentinoids for treatment. Unfortunately, the widespread use of gabapentinoid drugs has resulted in reports of misuse and abuse. Gabapentin addiction and abuse in the UK. In the UK, Gabapentin misuse and addiction have become a growing concern, with a noticeable increase in the number of deaths linked to Gabapentin since its introduction, with 913 cases between 2004 and 2020. Gabapentinoid abuse appears to be far more prevalent among current or past opioid abusers (one study identified a 1.1 and 0.5% rate of gabapentin and pregabalin abuse, respectively, among the general population aged 16–59 years in the UK, whereas studies of patients with opioid use disorders demonstrated much higher gabapentin (15–22%) and While gabapentinoids have licensed indications they also have a potential for misuse. For patients with a previous / current substance misuse problem, prescribers should make a careful and thorough assessment balancing potential benefits with risks. When gabapentin is taken alone and as prescribed, there is little potential for abuse or addiction. However, when a person takes gabapentin with other medications—such as muscle relaxants, opioids, or anxiety medications—it can produce a high. The effects of gabapentin intoxication have been variously described as: 4. Relaxation/sense of calm.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |