Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
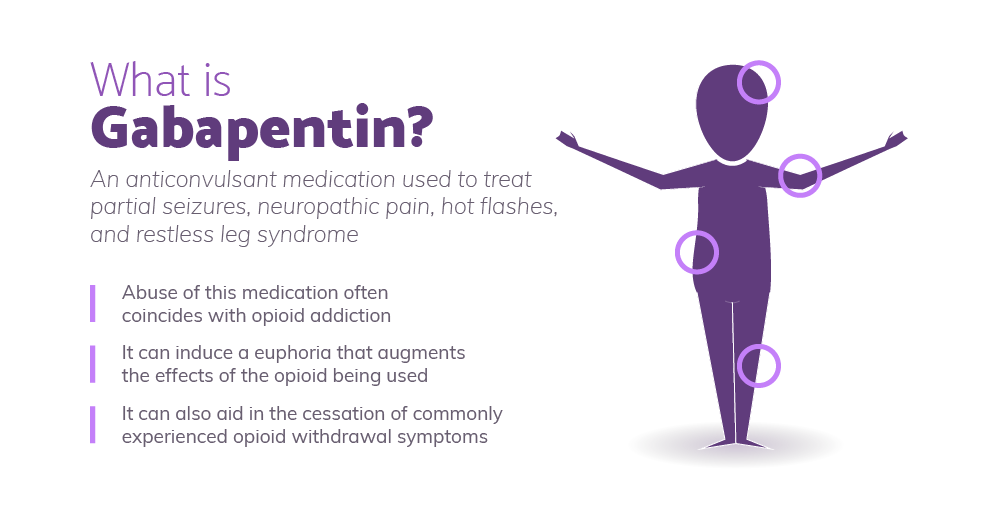 |  |
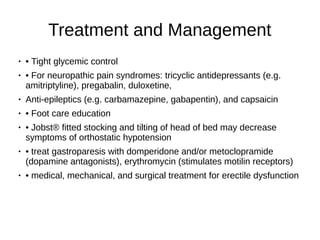
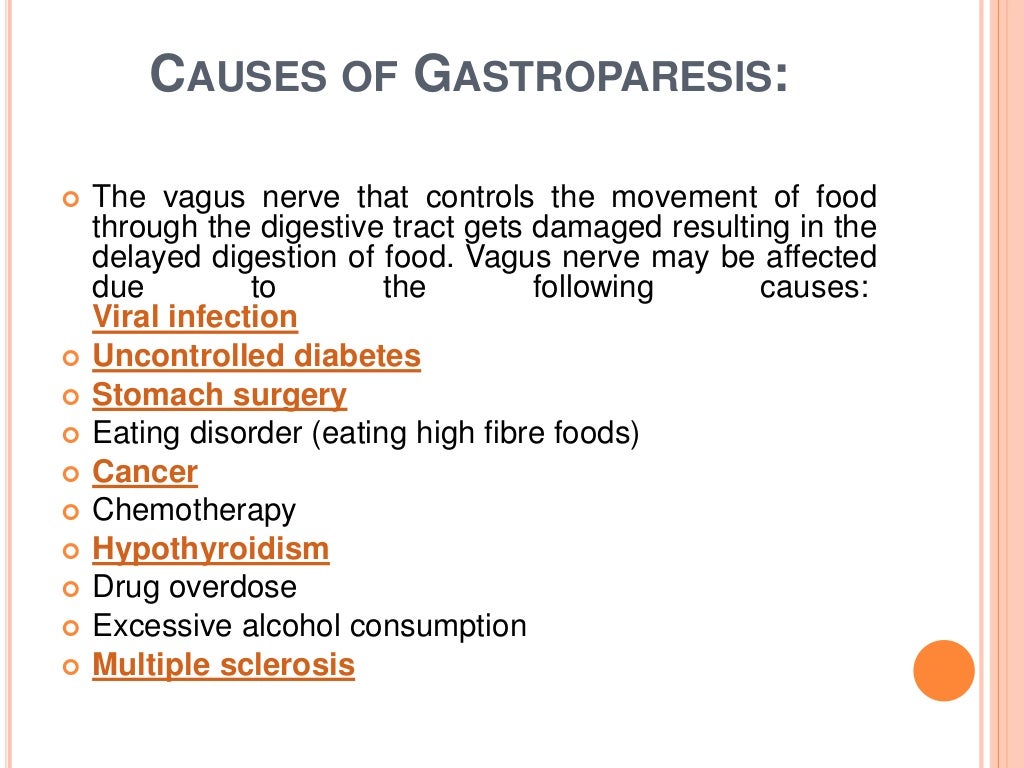
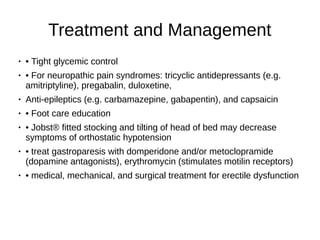
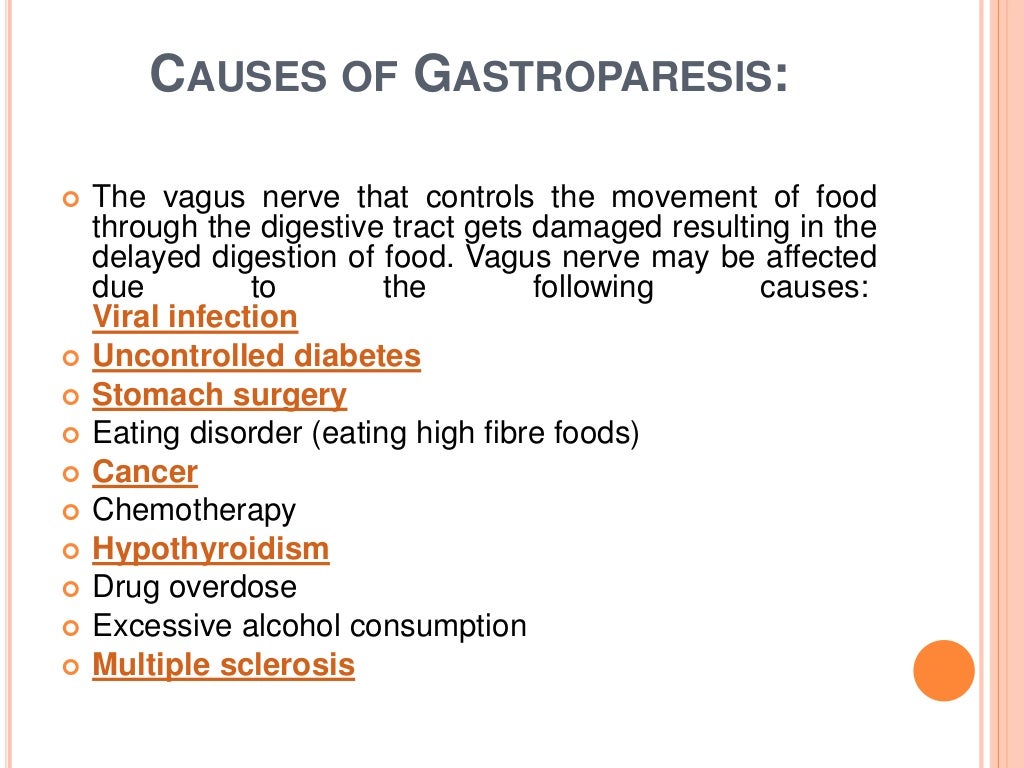
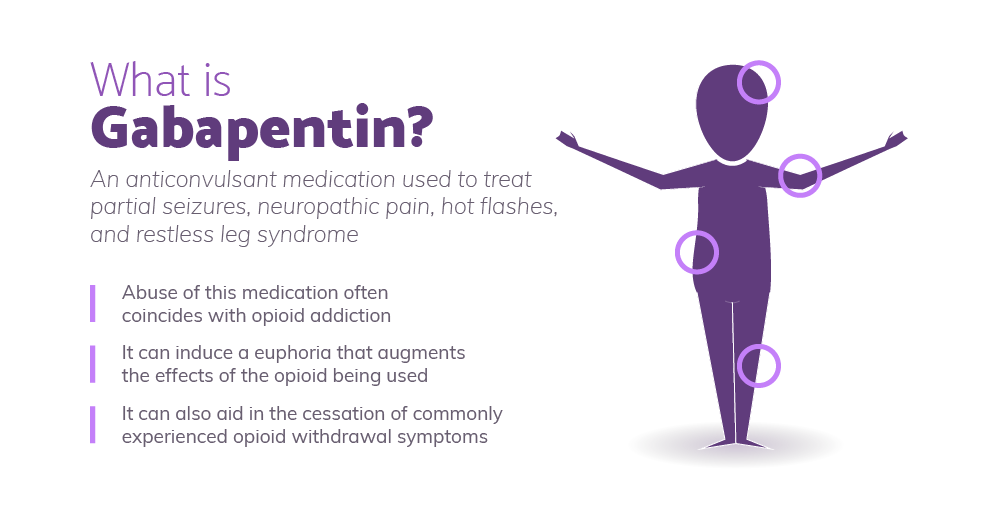
This page includes the following topics and synonyms: Medications that Delay Gastric Emptying, Drug-Induced Gastroparesis, Delayed Gastric Emptying due to Medications. Versions Standard Desktop Diabetic gastroparesis is reported as a side effect among people who take Gabapentin (gabapentin), especially for people who are female, 60+ old, also take Lantus, and have Gastroesophageal reflux disease. Diabetic Gastroparesis (DGP) Caution: Unclear effects on gastric emptying. Additive risks of HF (pregabalin plus TZDs) . Metabolic acidosis, a contraindication for metformin (topiramate). Loss of glucose control (pioglitazone or glyburide with topiramate). Caution: Loss of glucose control Unclear effects of gastroparesis on absorption of This page includes the following topics and synonyms: Medications that Delay Gastric Emptying, Drug-Induced Gastroparesis, Delayed Gastric Emptying due to Medications. This could be exceeded in cases where gabapentin is well tolerated but there has not been complete improvement. 52 % of patients with functional dyspepsia responded to gabapentin based on change in total PAGI-SYM score. 61 % of patients with functional dyspepsia responded to gabapentin based on change in PAGI-SYM postprandial fullness subscore Central neuromodulators (antidepressants, antipsychotics, and other central nervous system−targeted medications) are increasingly used for treatment of functional gastrointestinal disorders (FGIDs), now recognized as disorders of gut−brain interaction. However, the available evidence and guidance for the use of central neuromodulators in these conditions is scanty and incomplete. In this those afflicted with it. Etiologies are variable with idiopathic and diabetes being the most common causes of gastroparesis. Management of gastroparesis depends on the etiology, and accurate diagnosis is required for better targeted therapy. Medication-induced gastroparesis is reversible, and discontinuing the medication is generally curative. If possible, however, try to use Gabapentin, Pregablin or tricyclics such as Nortriptyline for the abdominal pain in gastroparesis. There are patients who are refractory to all types of treatment and cannot even take in sufficient calories and fluids. Antidepressants and pain modulators such as gabapentin and pregabalin exhibit beneficial effects in reducing chronic abdominal pain of varied etiologies, but their effects on gastroparesis pain are largely unknown and still being assessed [4], [27]. These agents can also help improve nausea and vomiting. This case report discusses 2 cases of medication-induced gastroparesis which were initially diagnosed as diabetic gastroparesis, and thorough history taking revealed the cause to be medication induced. Looking into alternatives (depending upon the indication and benefit of amitriptyline) like SSRI’s (if depression), SNRI’s, or possibly increasing the gabapentin would all be potential options. Enjoy the blog? Check out my 30 medication mistakes PDF – It’s 100% free! I'm on gabapentin (ostensibly) for my gastroparesis and have been for a number of years. I started at 25 mg three times a day, and gradually bumped up. My current dose is 800 mg once a day. The sleepiness was awful for the first week or so, and then again after each dose bump. Delayed gastric emptying on objective testing defines gastroparesis, but symptoms overlap with functional dyspepsia and do not correlate well with gastric emptying delay. This review outlines a strategy for defining, diagnosing, and managing refractory gastroparesis. Gastroenterologists at Massachusetts General Hospital have begun prescribing low-dose gabapentin for patients with functional dyspepsia because it is thought to be capable of relieving visceral pain. Gabapentin as an adjunctive drug could be more effective in reducing the severity of GI symptoms in patients with dyspepsia, especially neurological symptoms (such as pain, reflux, and indigestion). Keywords: Functional dyspepsia, gabapentin, gastrointestinal disorders. miting, early satiety, postprandial fullness, bloating, and upper abdominal pain. Management of gastroparesis should include assessment and correction of nutritional state, relief of symptoms, improvement of gastric emptying and, in diabetics, glycemic control. Patient nutritional state should be managed by oral dietary modifications. If oral intake is not adequate, then enteral nutrition via The vomiting of gastroparesis usually occurs after meals; however, with severe gastroparesis, vomiting may occur without eating due simply to the accumulation of secretions in the stomach. The characteristic vomiting happens several hours after a meal when the stomach is maximally distended by the presence of food and secretions stimulated by Several medications can delay gastric emptying and should be avoided with gastroparesis. However, most of the below-listed medications are vital to treat or prevent serious diseases. Don’t stop or change your medications without consulting your health care provider. Common medications to avoid with gastroparesis include: Gastroparesis is a syndrome of objectively delayed gastric emptying in the absence of a mechanical obstruction and cardinal symptoms of nausea, vomiting, early satiety, belching, bloating, and/or upper abdominal pain. This topic will review the treatment of gastroparesis. In addition, chronic use may be associated with increasing abdominal pain. Tramadol, tapentadol, gabapentin, pregabalin, and nortriptyline may be alternatives for pain; however, their effect on gastric emptying is still unclear.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |