Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |
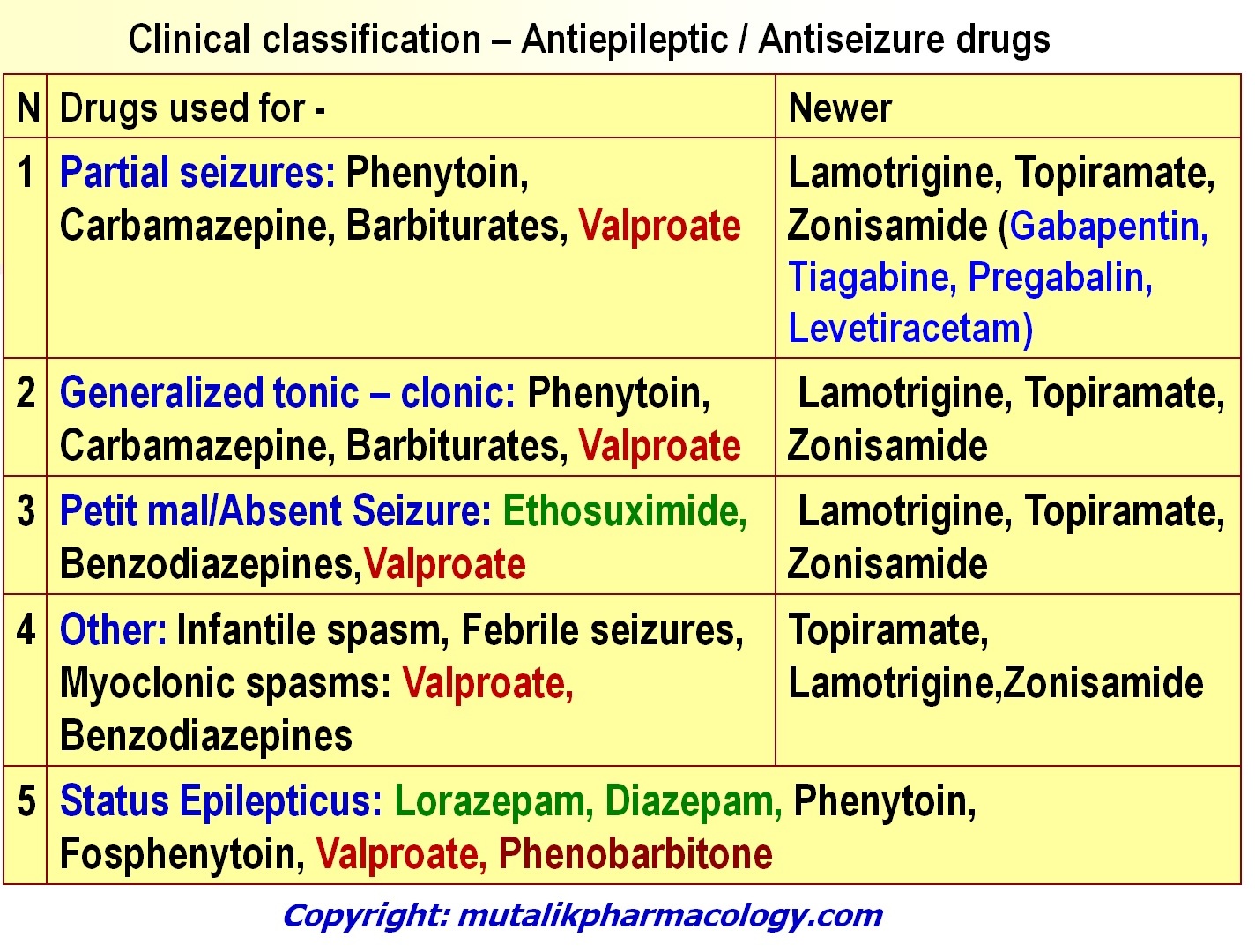
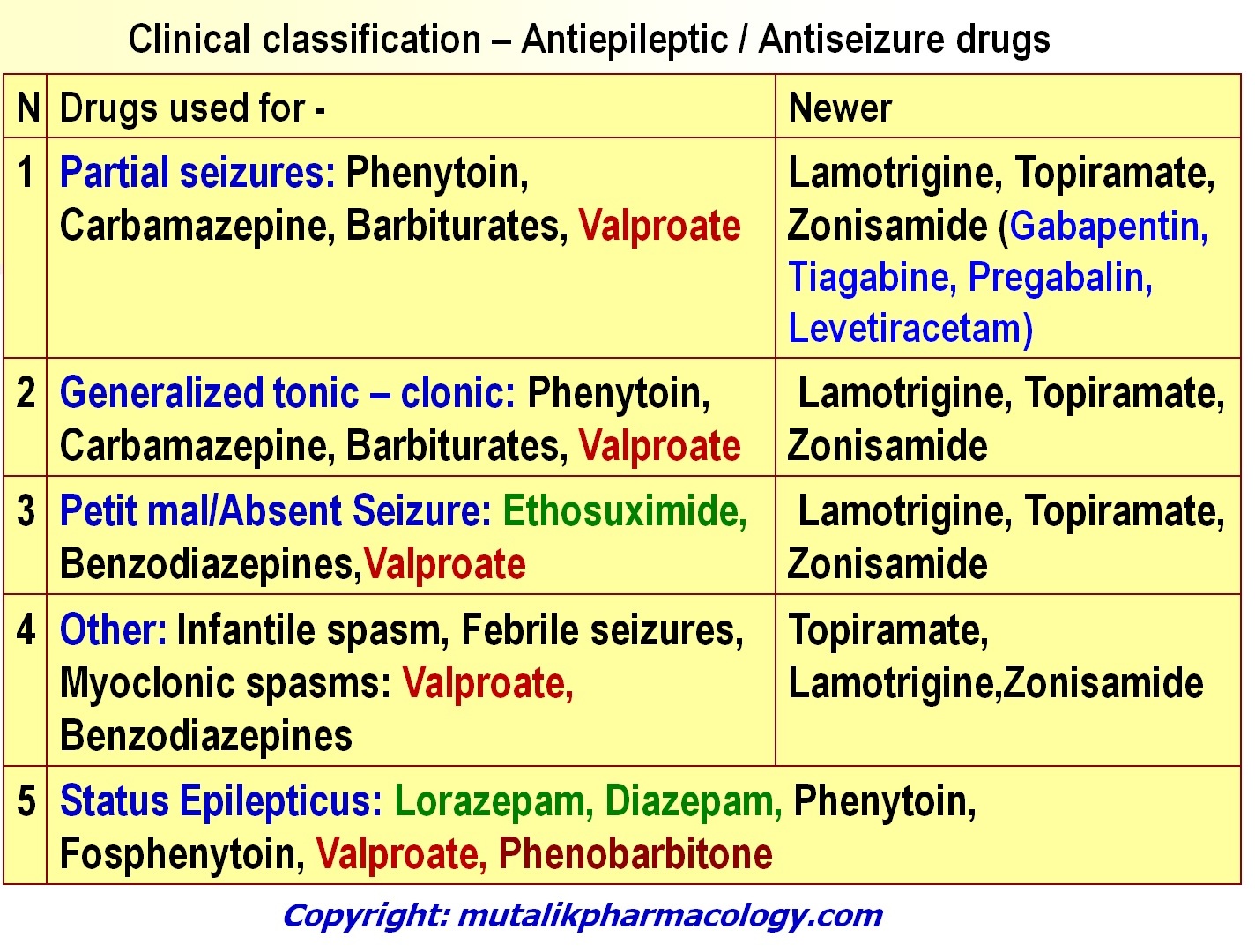
Beta-lactam antibiotics, including penicillins, cephalosporins and carbapenems, interact with the GABAA receptor to interfere with the inhibitory effects of GABA in a concentration-dependent manner.2 Correspondingly, they have dose-dependent effects on the seizure threshold.3,4 However, the CNS penetration of penicillins and cephalosporins is re Certain medications can lower your seizure threshold and make you more likely to have a seizure. Medications commonly associated with lowering the seizure threshold include bupropion and clozapine (Clozaril). We often associate seizures with epilepsy — a brain disorder that causes seizures. Gabapentin is a Pfizer-made medication for focal aware and impaired seizures. For more information, visit the Epilepsy Foundation online. The AAN (2018) 19 guideline states that gabapentin may be considered to decrease seizure frequency in patients aged 60 years or older with new-onset focal epilepsy. Gabapentin is regarded as safe and tolerable with a promising pharmacokinetic profile and an extensive therapeutic index. 10 Also, gabapentin have been approved in Japan as adjunctive drug therapy for medically intractable seizures. 4. Epilepsy is a common yet heterogeneous disease. As a result, management often requires complex decision making. The ultimate goal of seizure management is for the patient to have no seizures and no considerable adverse effects from the treatment. Antiepileptic drugs are the mainstay of therapy, with more than 20 medications currently approved in the United States. Antiepileptic drug selection The results of the overall efficacy analysis showed that gabapentin reduced seizure frequency when used as an add‐on AED in people with drug‐resistant focal epilepsy. Drugs with potential to lower the seizure threshold are numerous and diverse. Whether they contribute to clinically overt seizures depends on the dosage in which they are taken, the time-course of their effects and the susceptibility of the patient. Crucially, however, their contribution to seizure risk is potentially modifiable. People with epilepsy tend to have a lower seizure threshold, meaning they’re more likely to have seizures. Some activities, conditions, and medications can lower this threshold. A seizure These neurons probably are an integral component of the thalamocortical circuits associated with absence seizures, a subtype of generalized seizures associated with brief episodes of staring and a characteristic three-per-second spike and wave pattern on the electroencephalogram (EEG) . CONTENTS Getting started: (1) Initial approach to status (2) After the dust has settled Causes Diagnosis & definition Definition of status epilepticus Seizure mimics Differentiation from pseudoseizure Treatment overview Initial treatment Benzodiazepine Hypoglycemia, hyponatremia, and thiamine deficiency Conventional antiseizure medication Neurolytic intubation Subsequent management NORSE may occasionally make seizures worse, either idiosyncratically when being introduced, or if the dose is excessive. Table 1 shows some medications which may provoke seizures by lowering the seizure threshold, rather than by interacting with antiepileptic drugs. We do not know how often seizures occur because a drug has altered the seizure threshold. Drugs to avoid in patients with seizures - Although the list of medications that lower seizure threshold is huge, most of these medications cause seizures only in rare occasions. - Example; all cephalosporins have the potential of inducing seizures, however only cefepime was found to be commonly implicated and Lertxundi et al7 reported a 3.2-fold increased risk of seizure with SGAs in comparison with first-generation antipsychot-ics (FGAs) (95% confidence interval [CI], 2.21 to 4.63), which went down to 2.08 (CI, 1.39 to 3.12) once clozapine was excluded. However, as the authors of both studies noted, Some agents may lower the seizure threshold, but Table 1 shows some medications which may provoke seizures by lowering the seizure threshold, rather than by interacting with antiepileptic drugs. We do not know how often seizures occur because a drug has altered the seizure threshold. In relation to Pregabalin (Lyrica), Gabapentin (Neurontin), Valproate (Epilim) and other anti-convulsants there is little safety data available at the moment. A lack of evidence does not imply that co-administration of these dugs with Paxlovid is safe. Drugs that lower the seizure threshold 5 A W Hitchings therapeutic doses. 39 In contrast to the clinical trial data, observational studies using large population databases have found an increased risk of seizures in association with most antidepressant drugs. 40,41 In a Some clinicians discontinue medication for the management of absence seizures when the patient has been seizure-free for 2 years and the EEG is normal; for febrile seizures when the child is 6 years old or seizure-free for 2 years, or after 30 months in otherwise healthy children who do not experience any complex seizures or sequelae after Trimethylxanthine, in much lower doses, was also documented to lower the convulsive threshold in some seizure models. For instance, the seizure threshold was decreased in rats following acute or chronic administration of caffeine (at 50 or 80 mg/kg) in pentylenetetrazol-induced seizures [ 16 ]. Gabapentin may be considered to decrease seizure frequency in patients aged 60 years or older with new-onset focal epilepsy. Supporting evidence: One double-blind randomized study compared efficacy and tolerability of gabapentin, lamotrigine, and carbamazepine in patients aged 60 years or older.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |