Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
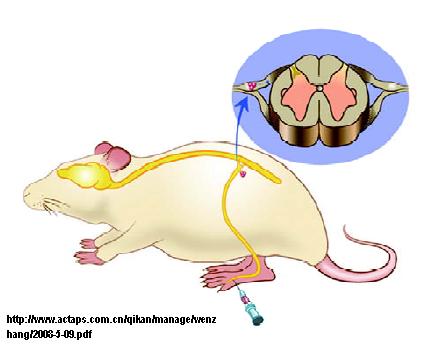
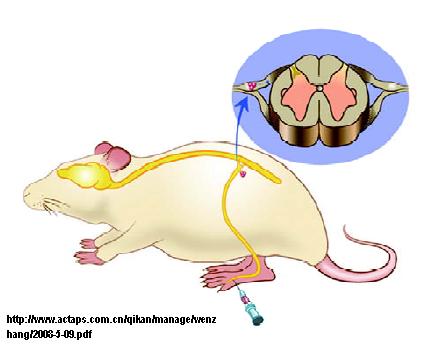
What is Vagal Neuropathy? Vagal neuropathy comes from the vagus nerve. The vagus nerve is the nerve in the throat and vagal neuropathy is in relation to the nerve not functioning correctly and sending false signals to the brain. Can Vagus Nerve Cause Chronic Cough? Yes damage to the vagus nerve can cause a chronic cough, tickle in throat and Leicester cough monitor trace from case 1. Schematic shows induced cough event during stimulation of the external auditory meatus in case 1. The patient was treated for sensory vagal neuropathy with gabapentin 1,800 mg/day for 1 month. Consolidation among different afferent branches of the vagus nerve is needed to bring about cough. A general, widely accepted view is that the chronic increase in the sensitivity of the cough reflex is associated with inflammatory hypersensitivity such as from gastro-esophageal reflux disease. Vagal and/or glossopharyngeal neuropathies, however, are relatively rare conditions that may present together. 8 Glossopharyngeal neuropathy is characterized by paroxysms of lancinating or burning pain in the oropharynx, whereas vagal neuropathy presents similarly but can also include symptoms of vocal cord dysfunction, such as hoarseness. Vagus nerve stimulation (VNS) can modulate vagal activity and neuro-immune communication. Human and animal studies have provided growing evidence that VNS can produce analgesic effects in addition to alleviating refractory epilepsy and depression. Gabapentin at doses of 1800 mg to 3600 mg daily (1200 mg to 3600 mg gabapentin encarbil) can provide good levels of pain relief to some people with postherpetic neuralgia and peripheral diabetic neuropathy. Such cases provide insight into its mechanism. It behaves like vagal or glossopharyngeal neuralgia, but instead of pain, the nerve damage or dysfunction causes an intermittent, abrupt-onset sensation that initiates the coughing. In general, the sensation itself is virtually the same each time, though its perceived urgency may vary. Gabapentin treatment of patients with chronic cough showed superior efficacy and a good safety record compared with placebo or standard medications. Additional randomized and controlled trials are needed. Keywords: Gabapentin, Cough, Treatment, Review Literature as Topic, Safety. A vagal neuropathy can also affect other motor branches of the vagus nerve, resulting in paresis or paralysis of the vocal folds, paradoxical vocal fold movement (PVFM), or other sensory branches inducing chronic cough, throat tickle, globus, sore throat, laryngeal paresthesia and laryngospasm. But after a while, the neuropathy medication doesn’t work anymore; because the reflux is still irritating the nerve, which is the reason for the neuropathy. If you don’t treat the triggering problem and you just treat the neuropathy, eventually the neuropathy medicine is not going to work because the reflux is still happening and continuing The presence of vocal fold motion asymmetry (VFMA) is associated with a favorable response to gabapentin therapy in patients with vagal neuropathy (VN)-related chronic cough, according to That’s right. Just wanted a disclaimer for anyone considering Gabapentin as a quick fix for vagus nerve dysfunction. Even though it’s a close analog, it is not safe long term. And for the record, Gabapentin also has no affinity for gaba or benzo receptors. It’s indirect action on gaba comes from its calcium channel interactions. Vagal neuropathies (“sick-nerve syndromes”) can affect the voice; and symptoms include voice change, vocal fatigue, effortful phonation, loss of singing power and pitch-range, and odynophonia (voice-use pain). In addition, vagal neuropathies can cause nerve pain in the throat, chest, and back. Vagus nerve damage by injury or infection can result in neurogenic (sick-nerve) symptoms. This post pertains to Dr. Koufman’s treatment schedule using amitriptyline and gabapentin for three specific syndromes; (1) painful speaking, aka voice-use pain or odynophonia; (3) chronic, sore (burning) throat, and neurogenic cough. Multiple neu-romodulating medications have been shown to be benefi-cial in the treatment of neurogenic cough, including amitriptyline, c-aminobutyric acid (GABA) analogs (gabapentin and pregabalin), and the GABA agonist bac-lofen.4 Although these medications may be effective in controlling neurogenic cough, they often require titration and some The purpose of this report is to review the clinical evidence on the efficacy, safety and guidelines for use of gabapentin in adults with neuropathic pain, and to examine evidence on the misuse or abuse of gabapentin and other drugs for neuropathic pain. Gabapentin was also beneficial in chronic cough patients with laryngeal sensory neuropathy . There is evidence that amitriptyline and gabapentin have central anti-nociceptive actions. Thus, relief from rectal pain by amitriptyline is associated with a reduction in pain-related responses in the anterior cingulate cortex in irritable bowel Gabapentin is effective for neuropathic pain with central sensitisation [21]. PRINT PDF.For most people with neurogenic cough, 800 mg. of gabapentin is not quite enough to knock out the cough. If you are on gabapentin 800 mg. (with 10 mg of amitriptyline) with insufficient benefit and no ill effects, contact your physician and escalate to gabapentin 300 mg. QID (4x/day)
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |