Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
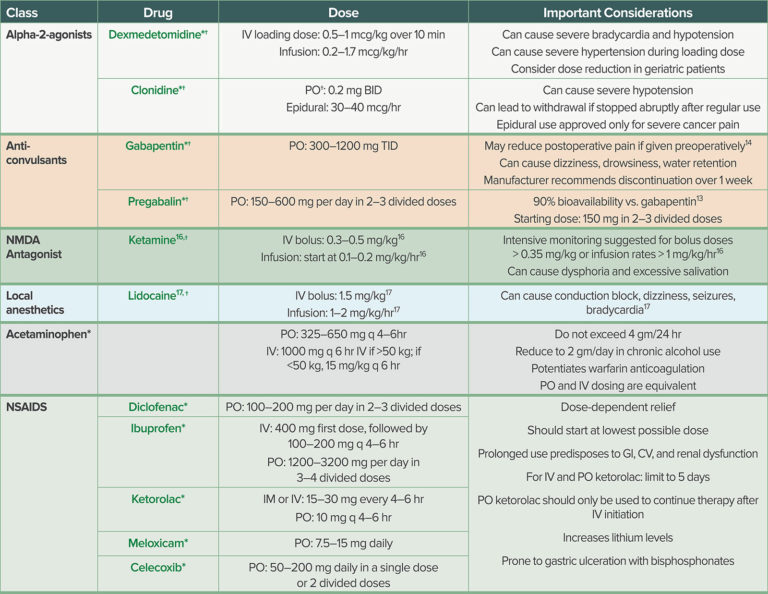
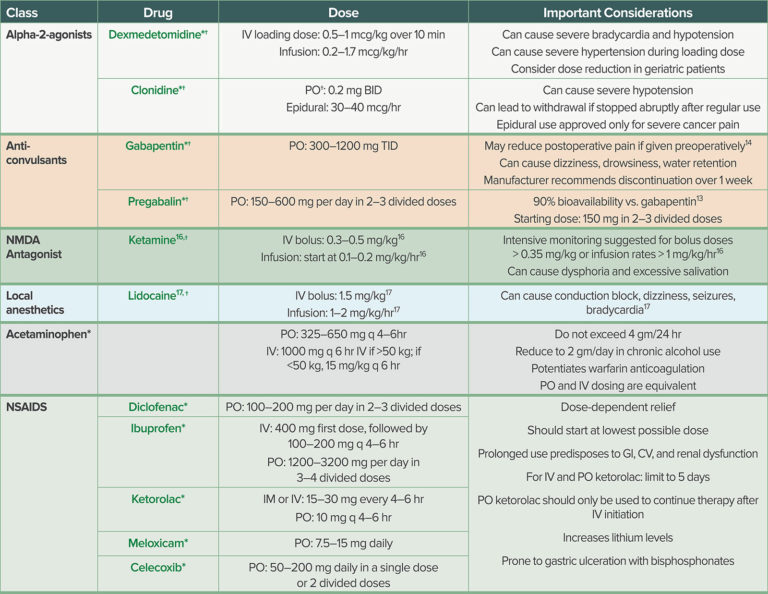
Post-operative gabapentin (600 mg) may be equally effective as a preoperative dose in decreasing PACU narcotic use. Concomitant administration of gabapentin as part of a multi-modal pain management strategy including narcotics, non-steroidal anti-inflammatory drugs (NSAIDS), and muscle relaxants does not improve pain scores. Gabapentin 250 mg is statistically superior to placebo in the treatment of established acute postoperative pain, but the NNT of 11 for at least 50% pain relief over 6 hours with gabapentin 250 mg is of limited clinical value and inferior to commonly used analgesics. Gabapentin 250 mg is not clinical Perioperative gabapentin may reduce the incidence and intensity of postoperative pain up to 6 months after otolaryngology, orthopedic, mastectomy, and abdominal/pelvic operations. 12-15 Professional guidelines advocate for perioperative administration of gabapentin as a component of multimodal analgesia, 16 but its efficacy in the context of Gabapentin 250 mg is statistically superior to placebo in the treatment of established acute postoperative pain, but the NNT of 11 for at least 50% pain relief over 6 hours with gabapentin 250 mg is of limited clinical value and inferior to commonly used analgesics. Weighted mean difference (WMD) for postoperative pain intensity (0–100 mm visual analogue scale) was −16.55 mm at 6 h and −10.87 mm at 24 h for treatment with a single preoperative dose of gabapentin 1200 mg. Cumulative opioid consumption at 24 h was also significantly decreased with gabapentin (WMD, −27.90 mg). Background: Perioperative pain treatment often consist of combinations of non-opioid and opioid analgesics, 'multimodal analgesia', in which gabapentin is currently used. The aim was to document beneficial and harmful effects of perioperative gabapentin treatment. They found that a single preoperative dose of 1200 mg effectively reduced postoperative pain and opioid consumption. Multiple doses of gabapentin preoperatively, and continued postoperatively, did not appear to reduce pain scores. Incidence of opioid adverse effects such as vomiting, and pruritus were lower in the gabapentin group. We evaluated the optimal preemptive dose of gabapentin for postoperative pain relief after single-level lumbar diskectomy and its effect on fentanyl consumption during the initial 24 hours in a randomized, double-blinded, placebo-controlled study in 100 patients with American Society of Anesthesiologists physical status I and II. l Affairs Committee met and discussed the perioperative use of gabapentinoids. t to take their regular dose on DOS and avoid ordering ad. ractions causing over sedation, it is OK if you don’t order the medicat. P et al. Use of Gabapentin for Perioper. tive Pain Contr. Straube S, Derry S, Moore RA, et al. Single dose oral gabapentin for established acute postoperative pain in adults. Cochrane Database Syst Rev 2010; 5:CD008183. [PMC free article] [Google Scholar] 20. Ho KY, Gan TJ, Habib AS. Gabapentin and postoperative pain—a systematic review of randomized controlled trials. Pain 2006; 126:91–101. Gabapentin is FDA approved for pain management of a limited number of neuropathic pain conditions; Gabapentin is widely used off-label for various chronic pain conditions and for the treatment of acute pain, making it now one of the most commonly described analgesic drugs; The liberal use of gabapentin for both acute and chronic pain management Weighted mean difference (WMD) for postoperative pain intensity (0–100 mm visual analogue scale) was −16.55 mm at 6 h and −10.87 mm at 24 h for treatment with a single preoperative dose of gabapentin 1200 mg. Cumulative opioid consumption at 24 h was also significantly decreased with gabapentin (WMD, −27.90 mg). tative pain scale.58 Secondary outcomes were postoperative subacute pain (defined as pain intensity during postopera-tive weeks 4 to 12); incidence of postoperative chronic pain (defined as pain lasting for 3 months or more); cumulative dose of opioids administered within 24, 48, and 72h after Gabapentin has been employed in a wide range of doses, but little is known about the optimal dose, providing the best balance between benefit and harm in postoperative pain treatment. The number of published, dose-finding gabapentin trials in postoperative pain treatment is limited, 1–11 and the results are inconsistent. Gabapentin 1,200 mg single dose pre-operatively. Gabapentin was associated with a statistically significant decrease in pain intensity at rest compared with placebo at 6 hours (6 RCTs; WMD -16.55 mm, 95% CI: -25.66, -7.44, p=0.0004) and 24 hours (3 RCTs; WMD -10.87 mm, 95% CI: -20.90, -0.84, p=0.03). Postoperative Pain The safety and efficacy of gabapentin in children undergoing surgery has been evaluated in several clinical trials. In 2010, Rusy and colleagues conducted a randomized double-blind placebo-controlled trial of gabapentin in 59 children 9 to 18 years of age undergoing spinal fusion.7 Scheduled gabapentin doses should be avoided in the post-operative period unless otherwise indicated for neuropathic pain Initial gabapentin doses for post-operative neuropathic pain should be limited to 300 mg per 24 hours Wean gabapentin over at least 2 weeks if receiving high doses (≥ 900 mg per 24 hours) for at least 4 weeks High dose Gabapentin caused a 35% reduction in total opioid consumption over the first 24 h following surgery (ratio of means 0.65, 95% CI 0.59 to 0.72), a significant reduction in postoperative pain at rest (in the first 24 h) and with movement (at 2 h, 4 h and 12 h), regardless of whether treatment effects were expressed as ratios of means or weighted m They used a gabapentin dose of 1.2 g per day treatment 1 hour before surgery and for 2 days after surgery and investigated its effect on postoperative acute pain. In this study, postoperative pain scores at 1, 2, and 3 days as well as the consumption of tramadol which was given as rescue analgesic were significantly lower in the gabapentin In this trustworthy systematic review, use of gabapentin for post-operative pain management was scrutinized. In summary, the quality of evidence for a clinically relevant benefit of gabapentin is low, and, importantly, harm may be present.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |