Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
.+The+patient+has+begun+to+hiccup+again+and+is+growing+increasingly+distressed+that+nothing+is+being+done.+The+patient%E2%80%99s+wife+has+repeatedly+come+to+the+nurse%E2%80%99s+station+demanding+action.+It+is+Friday+night+of+a+long+weekend+and+the+doctor+on+call+is+not+returning+the+page.+The+Doctor+had+made+is+very+clear+to+the+nurses%2C+that+he+is+not+to+be+called.+It+appears+to+be+a+doctor+oversight+that+it+was+not+renewed.+The+wife+persistently+demands+action+and+the+nurse+begins+to+cry.+The+head+nurse+intervenes..jpg) |  |
 |  |
 |  |
 | 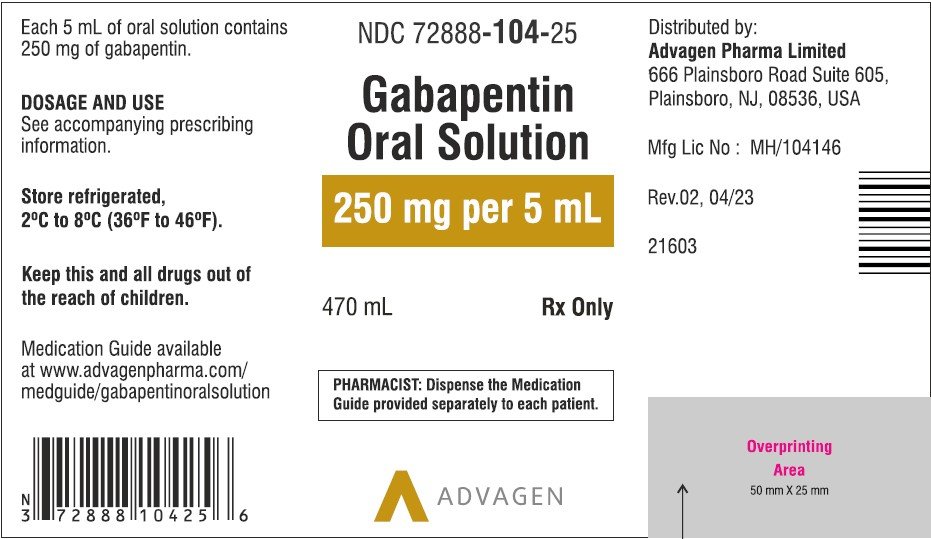 |
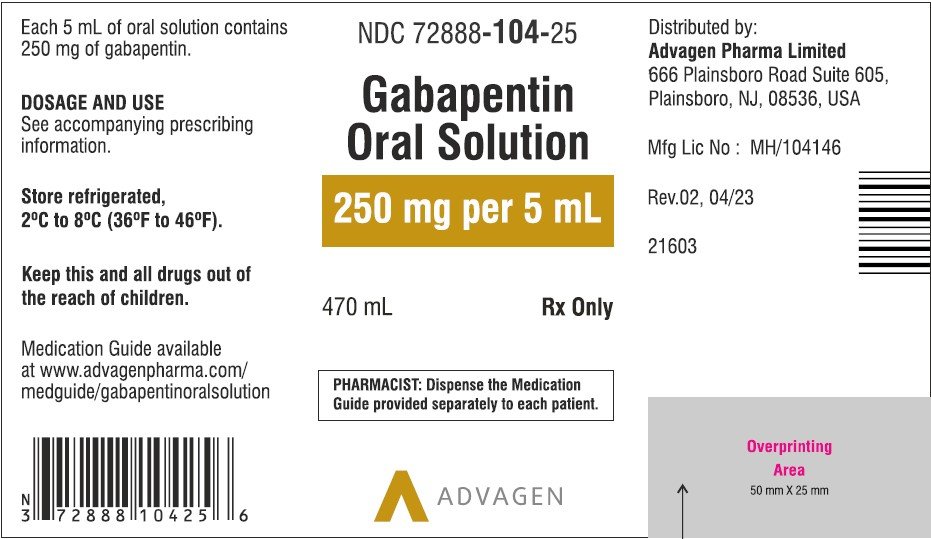
Stop feed and/or flush enteral tube with 15-30mL of water prior to drug administration. Ensure the patient is sitting up at an angle of at least 30 degrees to avoid reflux of medication or water. Give medication via enteral tube as directed by the guidance within the table. See below for guidelines on how to flush your feeding tube with water only. 1. Do NOT add medication directly to your tube feeding formula, unless specifically medication administration can be improved or maintained through the appropriate use of enteral alternatives such as gastrostomy tubes (GT), nasogastric tubes (NG), gastrostomy buttons (G-Buttons; GB), jejunostomy tubes (JT), and nasojejunal tubes (NJ). However, these routes present Feeding tubes are often clogged by poorly dissolved drugs, eliminating a vital route of administration to nutrients and subsequent medications. This document reflects a comprehensive review of all non-narcotic oral medications used at a cancer hospital for appropriateness for the feeding tube route. Pharmacist's Letter membership benefits include:. 12 issues every year — what you need to know and do, right now; Quick, practical reference charts and tools; Comprehensive CE library to meet license renewal and state requirements Any adverse effects, including problems with feeding tubes, should be reported to the prescriber and pharmacist immediately. 4 GENERAL PRINCIPLES When administering medication via enteral tube consideration needs to be taken regarding drug formulation, interactions with feed, type of tube, site of placement, and site of drug absorption. Introduction: Drug therapy can be com-plicated in hospitalized patients requir-ing an enteral feeding tube (EFT). Some medications may be given via an EFT while others are unsuitable for this form of administration. Inappropriate drug selection for EFT administration can cause potential toxicity, reduced efficacy, and tube obstruction. Administering drugs via feeding tubes is generally an unlicensed activity. There is little published data and most recommendations are theoretical and/or based on local policy. An alternative licensed option may therefore be preferable, e.g. rectal or parenteral formulations. Most medications that you normally take by mouth can be taken through your feeding tube. Medications must be in liquid form or crushed into a powder to prevent your feeding tube from getting clogged. Many medications come in a liquid form. Ask your healthcare provider about liquid forms if you take pills, tablets, or capsules. Gabapentin Rosemont Oral Solution is suitable for use with the following type of NG and PEG tubes: Ensure that the enteral feeding tube is free from obstruction before administration. 1. Flush the enteral tube with water, using the minimum fl ush volume required. 2. Administer the required dose of Gabapentin Rosemont Oral Solution with a %PDF-1.7 %âãÏÓ 112 0 obj > endobj xref 112 123 0000000016 00000 n 0000003281 00000 n 0000003486 00000 n 0000003527 00000 n 0000003562 00000 n 0000004020 00000 n 0000004126 00000 n 0000004241 00000 n 0000004349 00000 n 0000004463 00000 n 0000004571 00000 n 0000004686 00000 n 0000004791 00000 n 0000004906 00000 n 0000005013 00000 n 0000005128 00000 n 0000005235 00000 n 0000005350 00000 n Both nutrition and medication administration can be improved or maintained through the appropriate use of enteral alternatives such as gastrostomy tubes (GT), nasogastric tubes (NG), gastrostomy buttons (G-Buttons; GB), jejunostomy tubes (JT), and nasojejunal tubes (NJ). 2. Types of enteral feeding tube 4 3. Flushing enteral feeding tubes 9 4. Restoring and maintaining patency of enteral feeding tubes 15 5. Drug therapy review 23 6. Choice of medication formulation Alimemazine (Trimeprazine) tartrate25 7. The legal and professional consequences of administering drugs via enteral feeding tubes 38 8. Consistent with our study, Smith et al 5 found that gabapentin decreased pain during RT, but the dose was not increased beyond 900 mg for most patients because early pain relief occurred at this dose; most patients in our study tolerated 3600 mg. Cook et al 6 found no benefit to using 1800 mg of gabapentin daily; patients receiving gabapentin feeding tubes with or without fundoplication.7 Drugs for chronic pain have demonstrated great promise in improving oral feeding outcomes in medi-cally complicated children.8,9 The nerve-stabilizing medication gabapentin has been used for chronic neuro-pathic pain10 and reduced irritability in neurologically We would like to show you a description here but the site won’t allow us. Many medications may be put into your PEG. Here are some important things you need to know: If any medications cannot be put in your PEG, your pharmacist may help you by reaching out to the healthcare provider that prescribed a medication to suggest another option. In addition, use of gabapentin for persistent pain in children with SNI resulted in a significant reduction of associated GI symptoms, including decreased emesis and retching, improved feeding tolerance, weight gain, and change from J-tube to G-tube feedings [17,20,21]. Multivariable competing risks analysis among cohorts receiving daily doses of gabapentin, 900 mg, 2700 mg, or 3600 mg (reference cohort). Adjusted for age, sex, performance status, body mass index, pretreatment feeding tube placement, primary disease site, cancer stage, and receipt of unilateral vs bilateral neck radiotherapy.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
.+The+patient+has+begun+to+hiccup+again+and+is+growing+increasingly+distressed+that+nothing+is+being+done.+The+patient%E2%80%99s+wife+has+repeatedly+come+to+the+nurse%E2%80%99s+station+demanding+action.+It+is+Friday+night+of+a+long+weekend+and+the+doctor+on+call+is+not+returning+the+page.+The+Doctor+had+made+is+very+clear+to+the+nurses%2C+that+he+is+not+to+be+called.+It+appears+to+be+a+doctor+oversight+that+it+was+not+renewed.+The+wife+persistently+demands+action+and+the+nurse+begins+to+cry.+The+head+nurse+intervenes..jpg) |  |
 |  |
 |  |
 |  |