Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 | 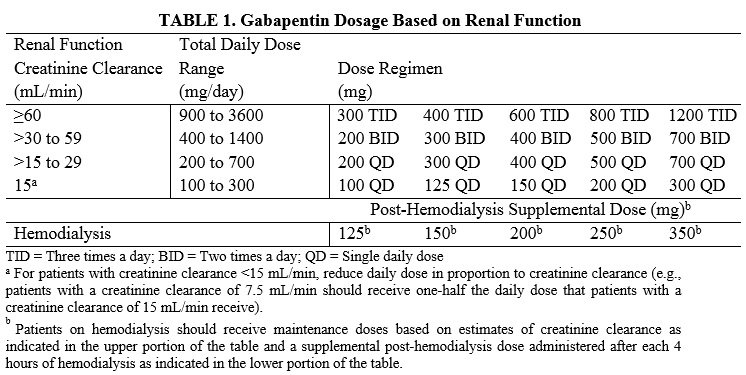 |
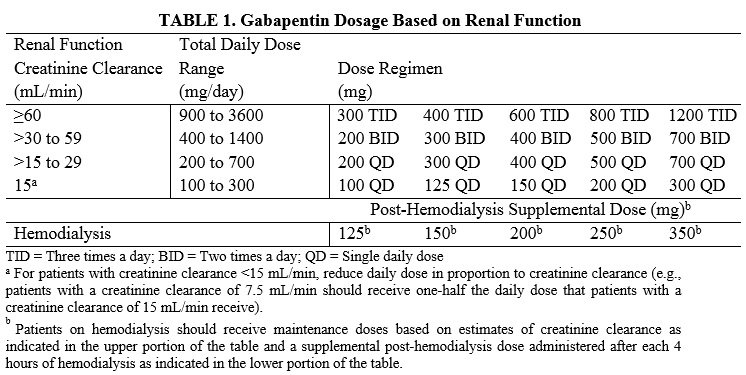
Background: Gabapentinoids (GPs) are frequently prescribed in individuals with chronic kidney disease (CKD); however, their exclusive renal elimination warrants dose adjustments to decrease risk of toxicity. This study evaluated GP prescribing patterns and whether excessive dosing was associated with increased incidence of gabapentinoid-related Challenges in pain management in patients with kidney disease. Pain assessment. This should start with assessment of a) pain severity using various standardized tools, most common of which is the numerical rating scale []; b) pathophysiologic evaluatio n into mechanism of injury and type of pain; c) psychosocial evaluation of co-occurring factors that contribute to pain or make treatment of Gabapentin is frequently used as an analgesic in patients with chronic kidney disease. Although gabapentin is well known for its favorable pharmacokinetics, it is exclusively eliminated renally, and patients with chronic kidney disease are at risk for toxicity. chronic kidney disease (CKD) patients as xerosis is prevalent in this population. • Lotions are not recommended (the higher concentrations of emulsifiers and stabilizers and the lower concentration of lipid in lotions can further worsen dry skin) • Other non-drug measures, e.g., minimizing the use Treating pain in the context of chronic kidney disease (CKD) is challenging because of altered pharmacokinetics and pharmacodynamics, with an increased risk of toxicity and drug adverse events in this population. The aims of this systematic review and meta-analysis were to assess the prevalence of analgesic use and establish the risk of analgesics-related adverse events, in patients with CKD. Gabapentin and pregabalin are commonly used for neuropathic pain in CKD patients but are not fully understood as this population remains excluded from efficacy and safety trials. Renal adjustments for the gabapentinoids are prodigiously recommended in the literature. Per Lexicomp, Gabapentin’s recommended dose in patients with renal impairment is as follows: CrCl >15 to 29 mL/minute: 200 to 700 mg once daily. CrCl 15 mL/minute: 100 to 300 mg once daily. In summary, gabapentin can be used in patients with stage 3 kidney disease, but only under careful medical supervision and with appropriate dosage adjustments. Never attempt to self-medicate or adjust dosages without consulting your doctor. The short answer is: yes, gabapentin can be problematic for individuals with kidney failure and chronic kidney disease (CKD). While gabapentin is often prescribed for pain management, particularly nerve pain, and sometimes for seizures, its primary elimination pathway is through the kidneys. Rationale & objective: Gabapentinoids are opioid substitutes whose elimination by the kidneys is reduced as kidney function declines. To inform their safe prescribing in older adults with chronic kidney disease (CKD), we examined the 30-day risk of serious adverse events according to the prescribed starting dose. Gabapentin dosing ranges from 100 to 3600 mg daily and pregabalin dosing is 25 to 600 mg daily. 1,2 Gabapentin and pregabalin exhibit greater than 90% kidney elimination and adjustments to dose and frequency are recommended for patients with chronic kidney disease (CKD). 1,2 For patients with a creatinine clearance (CrCl) below 60 mL/min, a CAPD :Probably dialysed. Dose as in GFR<15 mL/min. HD :Dialysed. Loading dose of 300–400 mg in patients who have never received gabapentin. Maintenance dose of 100–300 mg after each. HD : session and increase according to tolerability. HDF/high flux :Dialysed. Loading dose of 300–400 mg in patients who have never received gabapentin. Our literature search found only 2 population-based studies examining the association between gabapentin use and risk of toxicity in patients with CKD (our search strategy is shown in Table S2 and the results in Table S3). 11, 14 Only one study examined the risk of toxicity by initial gabapentin dose in new users, 14 and, in a subgroup analysis Many analgesics that are typically used in the non-CKD population should not be used among patients with advanced CKD (ie, estimated glomerular filtration rate [eGFR] <30 mL/min/1.73 m 2; including those on dialysis). This topic reviews the epidemiology, assessment of pain, and management of pain among patients with advanced CKD. Gabapentin is frequently used as an analgesic in patients with chronic kidney disease. Although gabapentin is well known for its well recieved pharmacokinetics, it is exclusively eliminated renally, and patients with chronic kidney disease are at risk for toxicity. The question of whether gabapentin is safe for cats with chronic kidney disease (CKD) is complex and requires careful consideration. The short answer is: it can be safe when used judiciously, but it’s not without risks and requires dosage adjustments due to the kidneys’ role in its elimination. Gabapentin is not absolutely contraindicated in kidney disease, but it demands meticulous management. The key to its safe use is careful dose adjustments, rigorous monitoring for toxicity, and an open dialogue with your healthcare provider. Patients with chronic kidney disease often receive inappropriately high gabapentin dosage for their kidney function, occasioning overt toxicity; advanced age and comorbidity predispose these patients for toxicity. Among 74,084 patients identified with CKD and a new prescription for gabapentin or pregabalin, 41% started at >300 or >75 mg/d, respectively. From this set of patients, a weighted study population with a size of 61,367 was generated. Diagnoses Associated with Gabapentin and Pregabalin Use. Gabapentin is Food and Drug Administration (FDA)-approved for the treatment of epilepsy and postherpetic neuralgia, 31 but it is commonly used off-label for other conditions, such as neuropathic pain, diabetic neuropathy, trigeminal neuralgia, and restless legs syndrome. 32 Pregabalin is
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |