Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
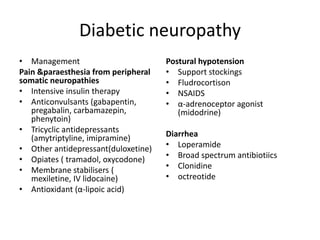
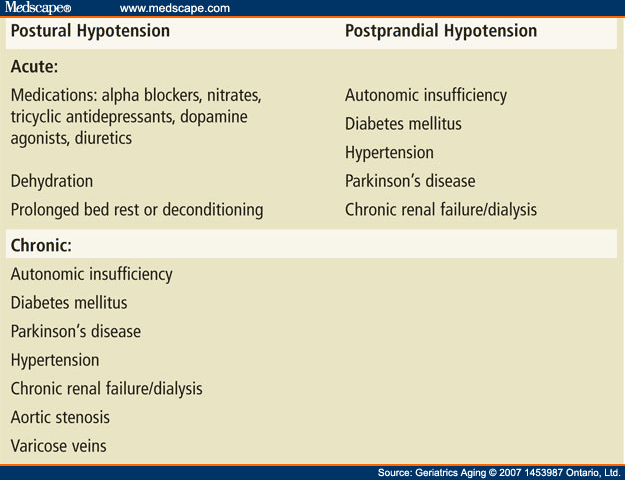
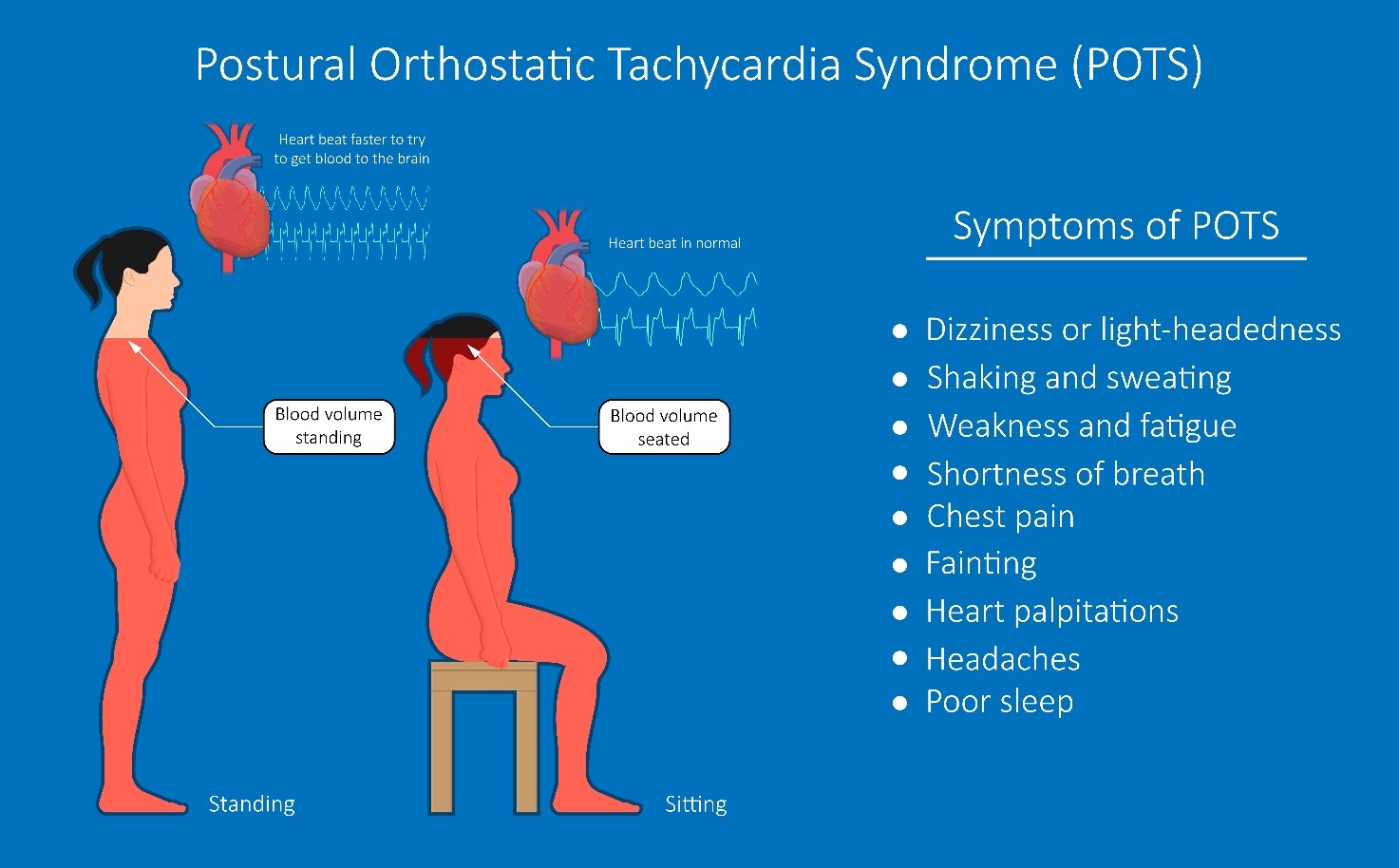
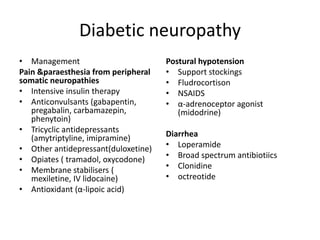
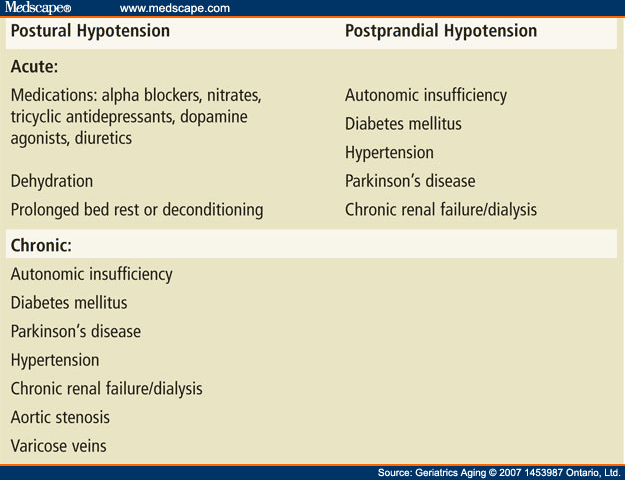
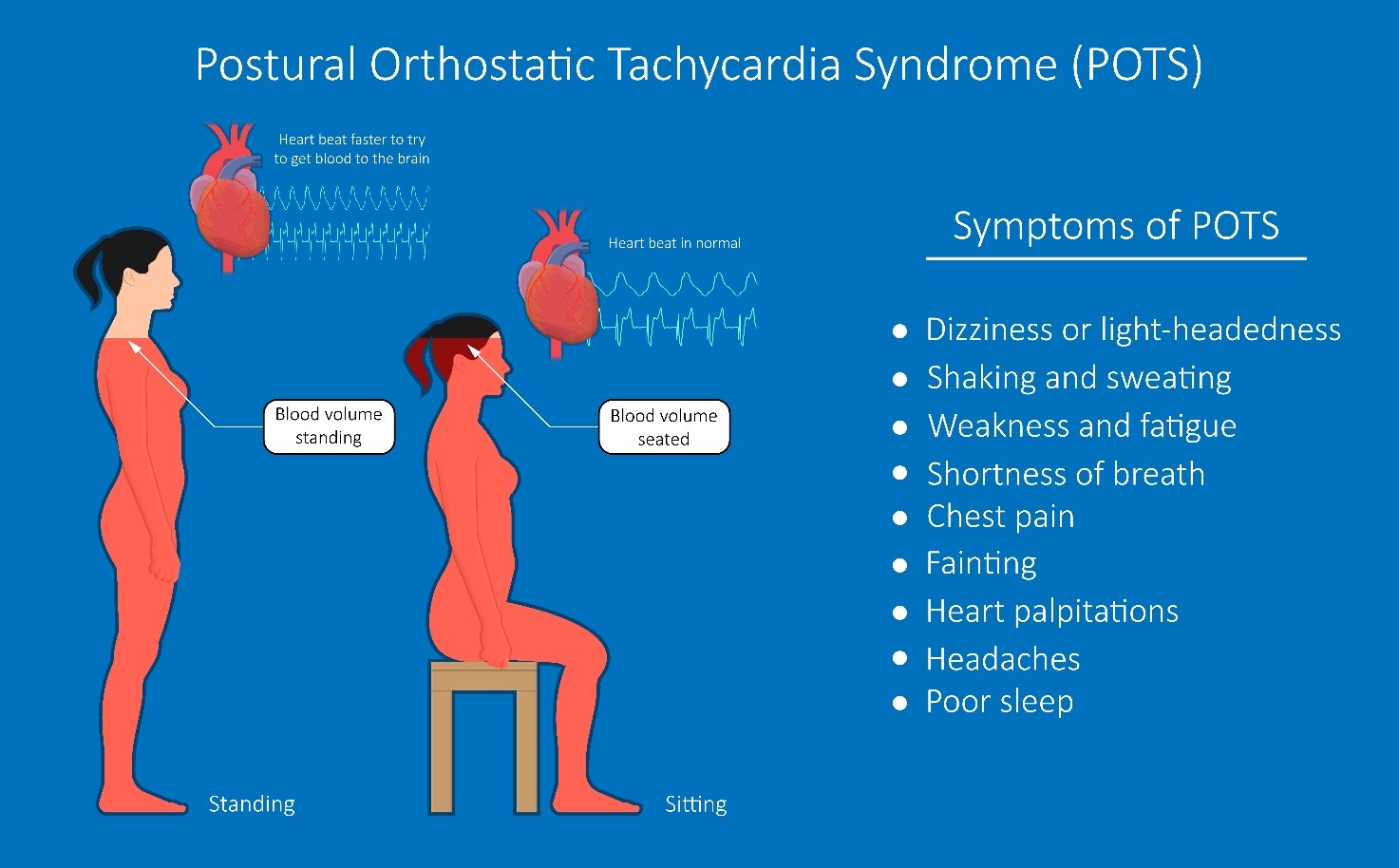
 |  |
Previous studies found that patients with neurogenic orthostatic hypotension can improve standing blood pressure and reduce symptoms of neurogenic orthostatic hypotension after a single administration of the selective NRI atomoxetine. How do you fix orthostatic hypotension? Orthostatic hypotension treatments vary by what’s causing it. Treatments may include: Treating a condition or disease that’s causing orthostatic hypotension. Changing the dose of a medication that causes orthostatic hypotension or switching to a different drug. Sitting up in bed if you’re on bed rest. Orthostatic hypotension (OH), defined as a reduction in systolic blood pressure (BP) of 20 mm Hg or diastolic BP of 10 mm Hg within 3 minutes of assuming an erect posture [1], is estimated to affect 30% to 70% of older adults [2] and is commonly associated with use of med-ications [3]. Orthostatic hypotension is a frequent cause of falls and syncope, impairing quality of life. It is an independent risk factor of mortality and a common cause of hospitalizations, which exponentially increases in the geriatric population. We present a management plan based on a systematic literature review and understanding of the underlying pathophysiology and relevant clinical pharmacology Orthostatic hypotension is a condition described by a significant reduction in blood pressure that typically occurs upon standing or assuming an upright posture. It may be asymptomatic or symptomatic and can be due to impaired autonomic reflexes or intravascular volume depletion. Abstract. Neurogenic orthostatic hypotension is a distinctive and treatable sign of cardiovascular autonomic dysfunction. It is caused by failure of noradrenergic neurotransmission that is associated with a range of primary or secondary autonomic disorders, including pure autonomic failure, Parkinson’s disease with autonomic failure, multiple system atrophy as well as diabetic and The overall rate is approximately 36 per 100,000 US adults and increases exponentially with age. 1 In patients older than the age of 75 years, the annual hospitalization rate related to orthostatic hypotension increases to 233 per 100,000 patients. 2 The prevalence of orthostatic hypotension in institutionalized patients ranges between 30% and Chronic orthostatic hypotension (OH) is a common, often underdiagnosed, disorder, defined by an excessive fall in blood pressure (BP) with standing. OH can be associated with postural lightheadedness, dizziness, fatigue, coat hanger pain, and, in extreme situations, syncope, falls, and injuries. A number of different drugs may either cause or contribute to orthostatic hypotension . Systemic illness that affects multiple organs (eg, cancer, diabetes mellitus, amyloidosis, and renal failure) may disturb autonomic function to a degree that orthostatic hypotension and syncope occur. Autonomic complaints are frequently encountered in clinical practice. They can be due to primary autonomic disorders or secondary to other medical conditions. Primary autonomic disorders can be categorized as orthostatic intolerance syndromes and small fiber neuropathies; the latter are associated with autonomic failure, pain, or their combinations. The review outlines orthostatic intolerance Data on chronic opioid treatment are limited, but hypotension, orthostatic hypotension, and syncope are commonly reported among potential adverse effects of most opioid analgesics, such as morphine, buprenorphine, fentanyl, oxycodone, and tapentadol [55•]. Yet, the mechanism underlying opioid-mediated hypotension still remains a matter of debate. Hypotension and orthostatic hypotension may contribute to fall risk, but evidence is inconsistent. There is no strong evidence indicating a specific class is preferred over others due to lower fall risk. However, with the possibility of orthostatic hypotension contributing to falls and strong evidence of Orthostatic hypotension (OH) is defined as a decrease in systolic blood pressure of more than 20 mmHg or a decrease in diastolic blood pressure of more than 10 mmHg after standing or tilting for 3 Several cardiovascular and psychoactive medications may alter the blood pressure response to standing, leading to drug-related orthostatic hypotension. This narrative review provides an overview on cardiovascular and non-cardiovascular medications potentially impairing orthostatic blood pressure. Orthostatic hypotension (OH) is defined as a persistent, consistent, orthostatic fall in systolic blood pressure of ≥20 mm Hg or diastolic pressure of ≥10 mm Hg by 3 minutes of standing up. 1 Acute, unexpected, episodic falls in blood pressure while standing, as in neurocardiogenic syncope, do not satisfy criteria for OH. Drug-induced orthostatic hypotension (OH) is common, and its resulting cerebral hypoperfusion is linked to adverse outcomes including falls, strokes, cognitive impairment, and increased mortality. The extent to which specific medications are associated with OH remains unclear. Gabapentin also reduces the release of glutamate in the dorsal horn of the spinal cord.14 These proposed mecha-nisms of action are supported by the limited efficacy of analogues of gabapentin which do not bind to the α 2δ-subunit.15,16 Gabapentin has also been shown to increase GABA levels in the CNS, which may account for its an- Orthostatic hypotension is defined as a decrease in blood pressure of 20 mm Hg or more systolic or 10 mm Hg or more diastolic within three minutes of standing from the supine position or on Oral and intravenous gabapentin can markedly attenuate blood pressure (BP) in hypertensive rats. The nucleus tractus solitarii (NTS) is the primary integrative center for cardiovascular control and other autonomic functions in the central nervous system. Neurogenic orthostatic hypotension (OH) is a disabling disorder caused by impairment of the normal autonomic compensatory mechanisms that maintain upright blood pressure. Nonpharmacologic treatment is always the first step in the management of this
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |