Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
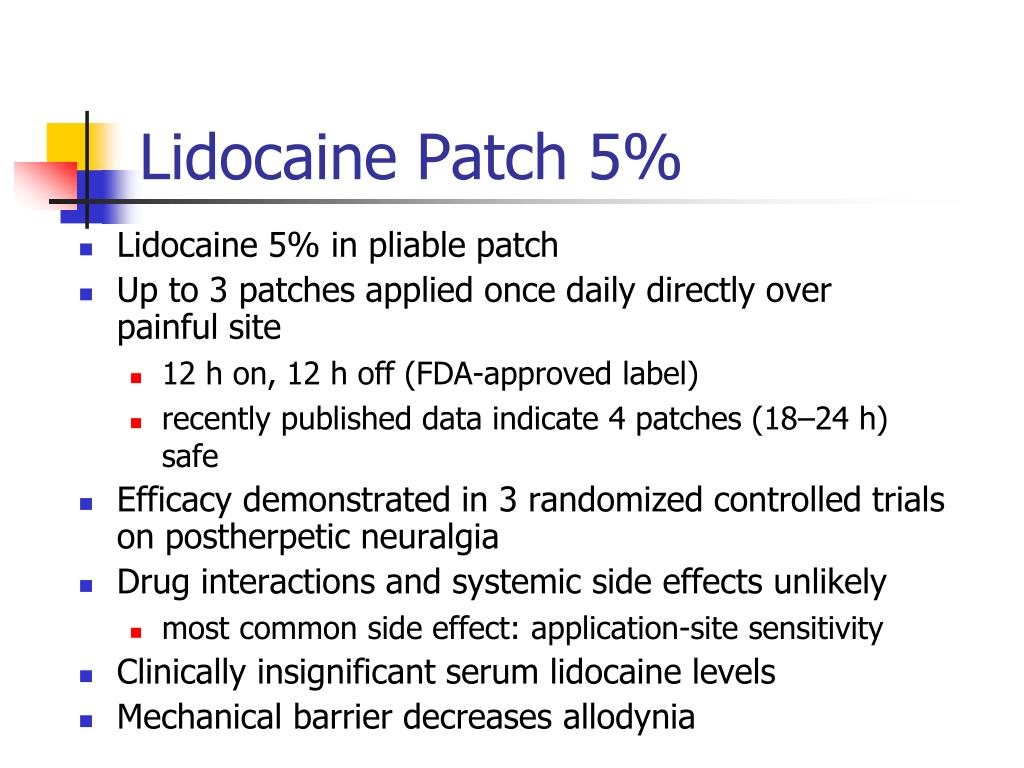
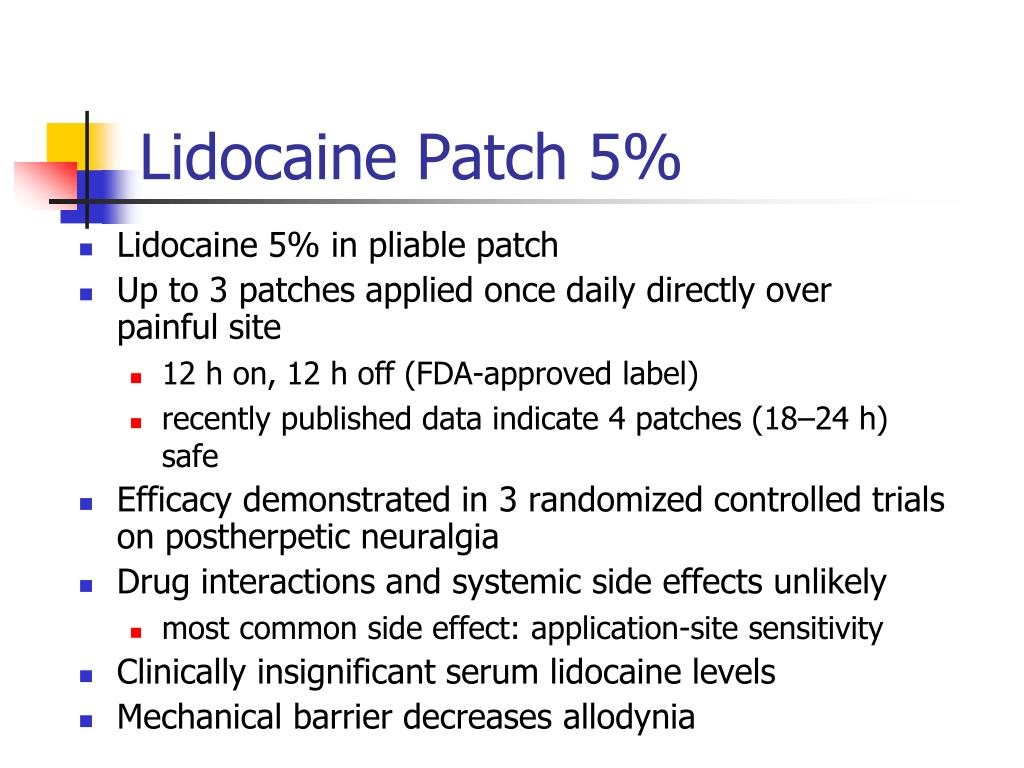
Gabapentin, when used topically, is not typically associated with the same level of systemic absorption as oral administration. However, caution should be exercised if the patient is taking other central nervous system (CNS) depressants, such as opioids, benzodiazepines, or alcohol, as there may be an additive effect on CNS depression. Topical analgesics are appealing to clinicians because their lack of systemic absorption results in limited adverse effects (AEs).¹ Other benefits of topical analgesics include direct access to target sites, convenience, ease of use, painless administration, and improved patient acceptance and adherence, all of which may reduce overall treatment costs.²⁻⁴ Most topical analgesics are Topical analgesics, especially compared to oral analgesics, are a newer and less commonly utilized modality in the treatment of chronic pain. While the majority of patients with chronic pain are treated with oral analgesics, there is increasing evidence topical analgesics in some cases may be as efficacious as those administered by the oral route with the added benefit of decreased systemic Increased absorption through compromised skin could increase the effectiveness of topical treatments, but it may also enhance potential systemic absorption and increased the risk of toxicity (Law et al., 2020). Topical application of Gabapentin offers localized pain relief with minimal systemic absorption. This targeted approach ensures effective pain management, particularly beneficial for patients requiring specific area-focused treatment, while minimizing the risk of systemic side effects commonly associated with oral medications. When formulated as a 10% topical gel, gabapentin is designed for localized treatment, potentially minimizing systemic absorption and reducing the likelihood of systemic drug interactions that are more common with oral administration. Topical delivery of gabapentin is desirable to treat peripheral neuropathic pain conditions whilst avoiding systemic side effects. To date, reports of topical gabapentin delivery in vitro have been variable and dependent on the skin model employed, primarily involving rodent and porcine models. However, it is important to consider that even when applied topically, some systemic absorption of gabapentin can occur, and therefore, interactions with other medications are still possible. Patients should be advised to inform their healthcare providers of all medications they are currently taking, including prescription drugs, over-the Topical delivery of gabapentin is desirable to treat peripheral neuropathic pain conditions whilst avoiding systemic side effects. To date, reports of topical gabapentin delivery in vitro have been variable and dependent on the skin model employed, primarily involving rodent and porcine models. In this study a variety of topical gabapentin formulations were investigated, including Carbopol Gabapentin 40 mg/g topical cream is a semisolid preparation designed for localized treatment or absorption of active ingredients through the skin. This formulation is primarily used to manage neuropathic pain and other conditions where localized delivery of gabapentin can provide therapeutic benefits. Topical administration allows for efficient, painless delivery of medications while reducing systemic adverse effects associated with parenteral or oral administration. Gabapentin completely diffused out of the three bases within 6 hours of application according to the Higuchi model. Flux of the drug appeared to be concentration-dependent with no permeation occurring at 1% strength. Skin concentrations increased with a longer 1-hour pre-treatment. Minimal skin and deeper tissue levels were found following a 4-hour pre-treatment. These results suggest that topical gabapentin may be antinociceptive in a rodent formalin model at specific doses and pre-treatment intervals. Like endogenous neurotransmitter (γ-aminobutyric acid [GABA]), topical gabapentin blocks calcium channels and N-methyl-d-aspartate receptors (NMDA) in peripheral nerves, 2 which results in neuropathic pain relief. Systemic absorption occurs with both oral and topical NSAIDs, but topical NSAID formulations produce only 2% to 8% of the peak serum concentration of oral NSAIDs. 52 Because of this, topical NSAIDs are associated with a lower risk of serious adverse effects. 52,71,76,86 Whereas topical NSAIDs are considered safe overall, they are not completely Since the total systemic absorption from the topical application is only 3–5% of the oral administration, systemic toxicity from topical NSAIDs is consequently rare . Previous studies have demonstrated that topical NSAIDs could reach sufficient therapeutic concentration; When applied topically, the concentration of ketoprofen was 30-fold systemic absorption seems to be minimal, further exploration of of topical gabapentin for vulvodynia.12 Furthermore, topical Topical administration of bupivacaine on mucous membranes or nonintact skin could enhance systemic absorption and potentially result in significant toxicity. From the FDA-approved label, serious adverse effects from oral administration of this API include cardiac arrest and respiratory depression. Gabapentin was nominated for vulvodynia via topical and vaginal cream (3-10%). It was also nominated to treat an unspecified medical condition, but the nominators said that it is generally used to treat pain. absorption • Drug concentration at the site of administration can be 30 fold higher than with an oral dose • Decreased potential for systemic side effects when targeting specific areas with a transdermal Sawynok J. Topical analgesics in neuropathic pain.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |