Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
.jpeg?w=828) |  |
 |  |
 |  |
 |  |
 |  |
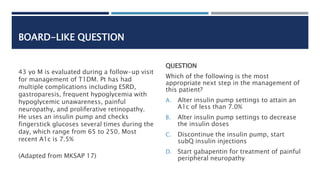
Central neuromodulators (antidepressants, antipsychotics, and other central nervous system−targeted medications) are increasingly used for treatment of functional gastrointestinal disorders (FGIDs), now recognized as disorders of gut−brain interaction. However, the available evidence and guidance for the use of central neuromodulators in these conditions is scanty and incomplete. In this Diabetic gastroparesis in Gabapentin; Expand to all the drugs that have ingredients of gabapentin: Diabetic gastroparesis and drugs with ingredients of gabapentin (50 reports) More studies by gender and age: Female: 0-1 2-9 10-19 20-29 30-39 40-49 50-59 60+ Male: 0-1 2-9 10-19 20-29 30-39 40-49 50-59 60+ Browse all side effects of Gabapentin: Gabapentin as an adjunctive drug could be more effective in reducing the severity of GI symptoms in patients with dyspepsia, especially neurological symptoms (such as pain, reflux, and indigestion). Keywords: Functional dyspepsia, gabapentin, gastrointestinal disorders. Drugs used to relieve abdominal pain in gastroparesis include nonsteroidal anti-inflammatory drugs such as ibuprofen and naproxen , low-dose tricyclic antidepressants such as amitriptyline (Elavil, Endep), drugs that block nerves that sense pain such as gabapentin , and narcotics such as tramadol and fentanyl . I'm on gabapentin (ostensibly) for my gastroparesis and have been for a number of years. I started at 25 mg three times a day, and gradually bumped up. My current dose is 800 mg once a day. The sleepiness was awful for the first week or so, and then again after each dose bump. Relief for gastroparesis symptoms: Gabapentin can provide relief for symptoms associated with gastroparesis, including nausea, vomiting, bloating, and abdominal pain. By targeting the nervous system, gabapentin helps to regulate the digestive process and improve gastric emptying, providing relief from these distressing symptoms. However, unlike the currently available literature, this report details the case of a two-month-old female with severe feeding intolerance, suspected gastroparesis, visceral hyperalgesia, and malnutrition without previous neurological conditions or cardiac surgery and the role of gabapentin in addressing her FTT. Gastroparesis is a syndrome of objectively delayed gastric emptying in the absence of a mechanical obstruction and cardinal symptoms of nausea, vomiting, early satiety, belching, bloating, and/or upper abdominal pain. This topic will review the treatment of gastroparesis. Gastroparesis is a syndrome characterized by delayed gastric emptying in the absence of any mechanical cause. While often associated with diabetes mellitus, most cases of gastroparesis are idiopathic. The purpose of the present paper is to review those afflicted with it. Etiologies are variable with idiopathic and diabetes being the most common causes of gastroparesis. Management of gastroparesis depends on the etiology, and accurate diagnosis is required for better targeted therapy. Medication-induced gastroparesis is reversible, and discontinuing the medication is generally curative. If possible, however, try to use Gabapentin, Pregablin or tricyclics such as Nortriptyline for the abdominal pain in gastroparesis. There are patients who are refractory to all types of treatment and cannot even take in sufficient calories and fluids. Gastroparesis can be a serious problem where the GI tract literally “slows down”. This issue is common in patients with diabetes. Bloating, abdomnial pain, nausea, vomiting, and a feeling of fullness are all possible symptoms of gastroparesis. There are also medications that can worsen gastroparesis. The case: KD is a 62 year old female who [] Gastroparesis is identified in clinical practice through the recognition of the clinical symptoms and documentation of delayed gastric emptying. Symptoms from gastroparesis include nausea, vomiting, early satiety, postprandial fullness, bloating, and upper abdominal pain. Delayed gastric emptying on objective testing defines gastroparesis, but symptoms overlap with functional dyspepsia and do not correlate well with gastric emptying delay. This review outlines a strategy for defining, diagnosing, and managing refractory gastroparesis. Treatment. Treating gastroparesis begins with finding and treating the condition that's causing it. If diabetes is causing your gastroparesis, your healthcare professional can work with you to help you control your blood sugar levels. Gastroparesis is characterized by symptoms suggesting retention of food in the stomach with objective evidence of delayed gastric emptying in the absence of mechanical obstruction in the gastric outflow. This condition is increasingly encountered in clinical practice. Gastroenterologists at Massachusetts General Hospital have begun prescribing low-dose gabapentin for patients with functional dyspepsia because it is thought to be capable of relieving visceral pain. Abstract. Gastroparesis (GP), a historically vexing disorder characterized by symptoms of nausea, vomiting, abdominal pain, early satiety, and/or bloating, in the setting of an objective delay in gastric emptying, is often difficult to treat and carries a tremendous burden on the quality of patients’ lives, as well as the healthcare system in general. This page includes the following topics and synonyms: Medications that Delay Gastric Emptying, Drug-Induced Gastroparesis, Delayed Gastric Emptying due to Medications. This case report discusses 2 cases of medication-induced gastroparesis which were initially diagnosed as diabetic gastroparesis, and thorough history taking revealed the cause to be medication induced.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
.jpeg?w=828) |  |
 |  |
 |  |
 |  |
 |  |