Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
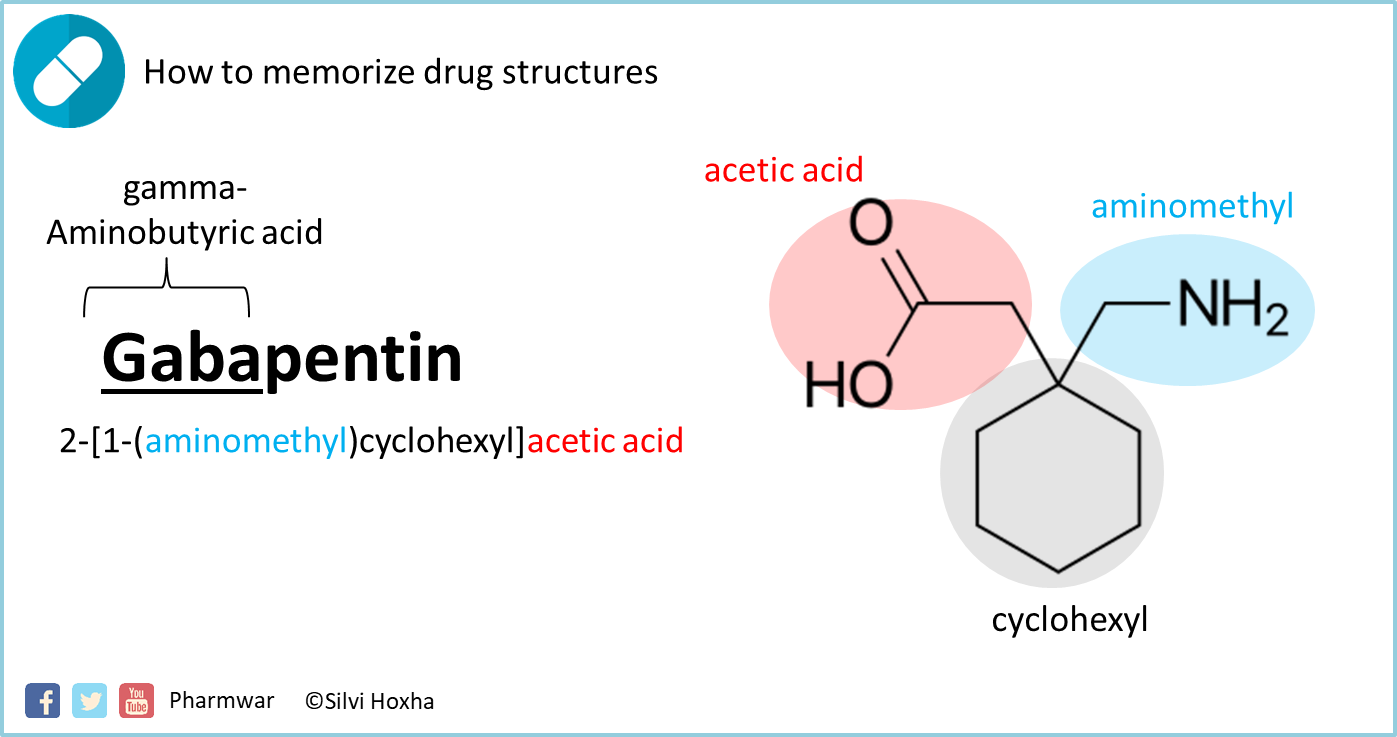 |  |
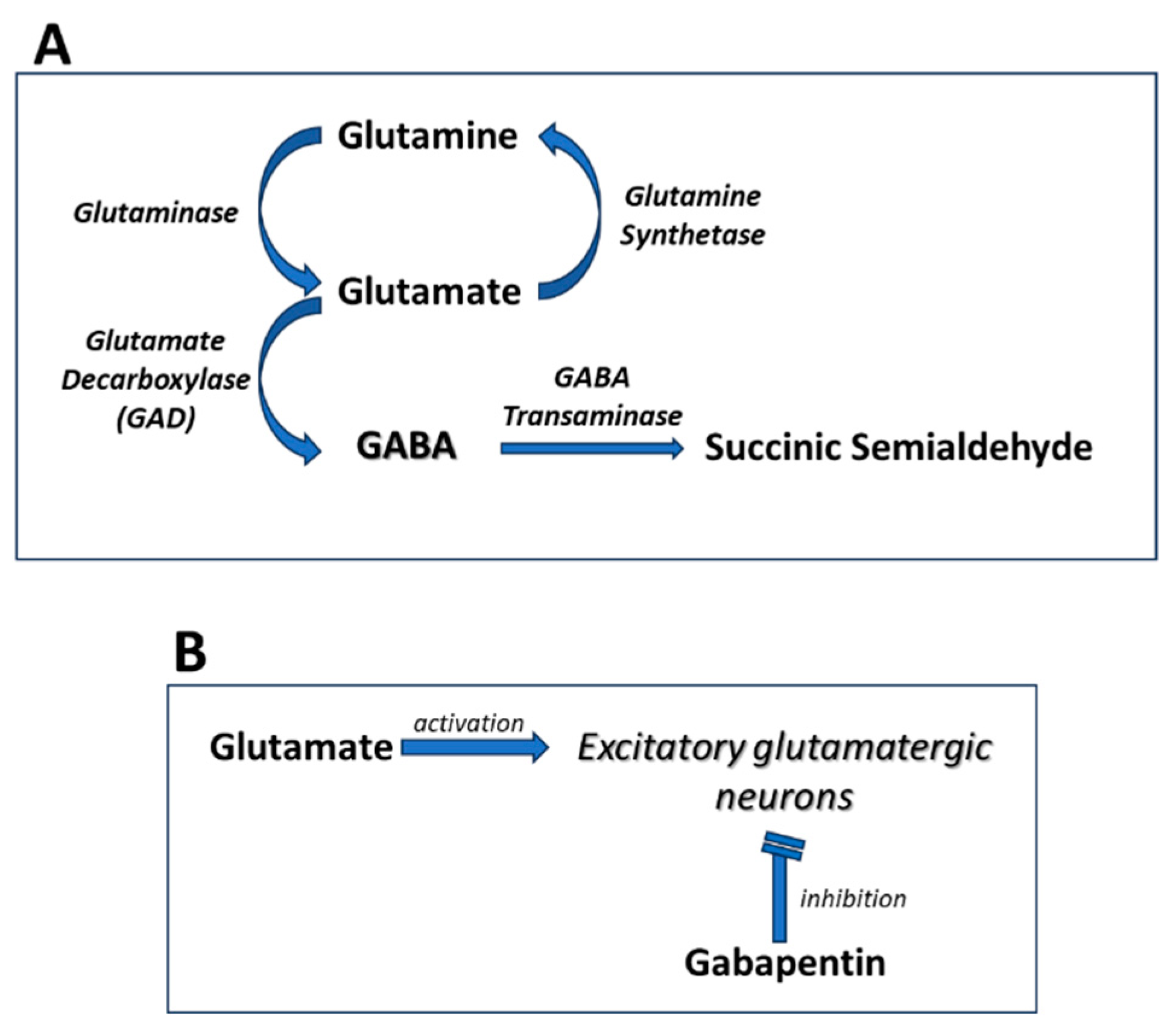
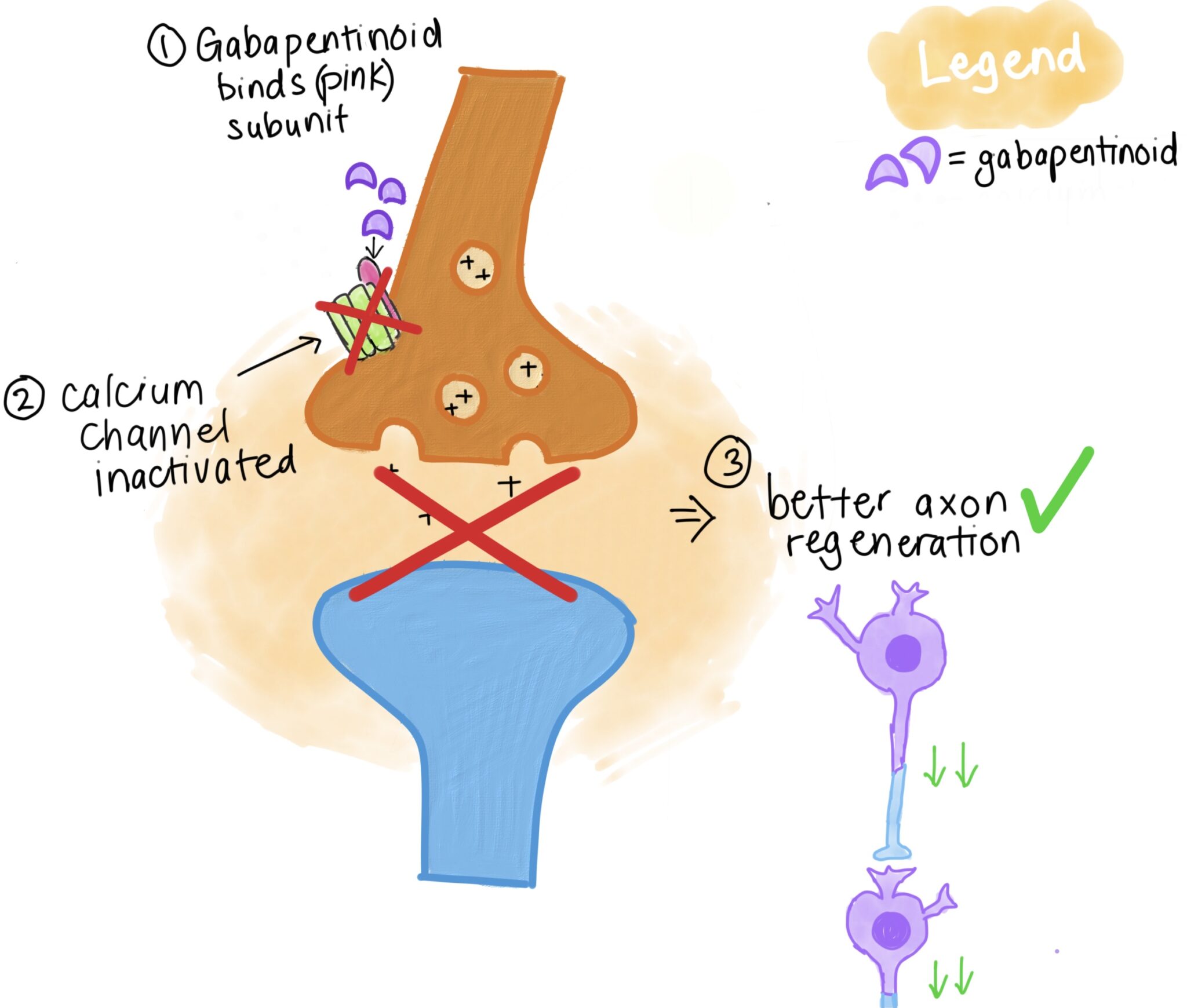
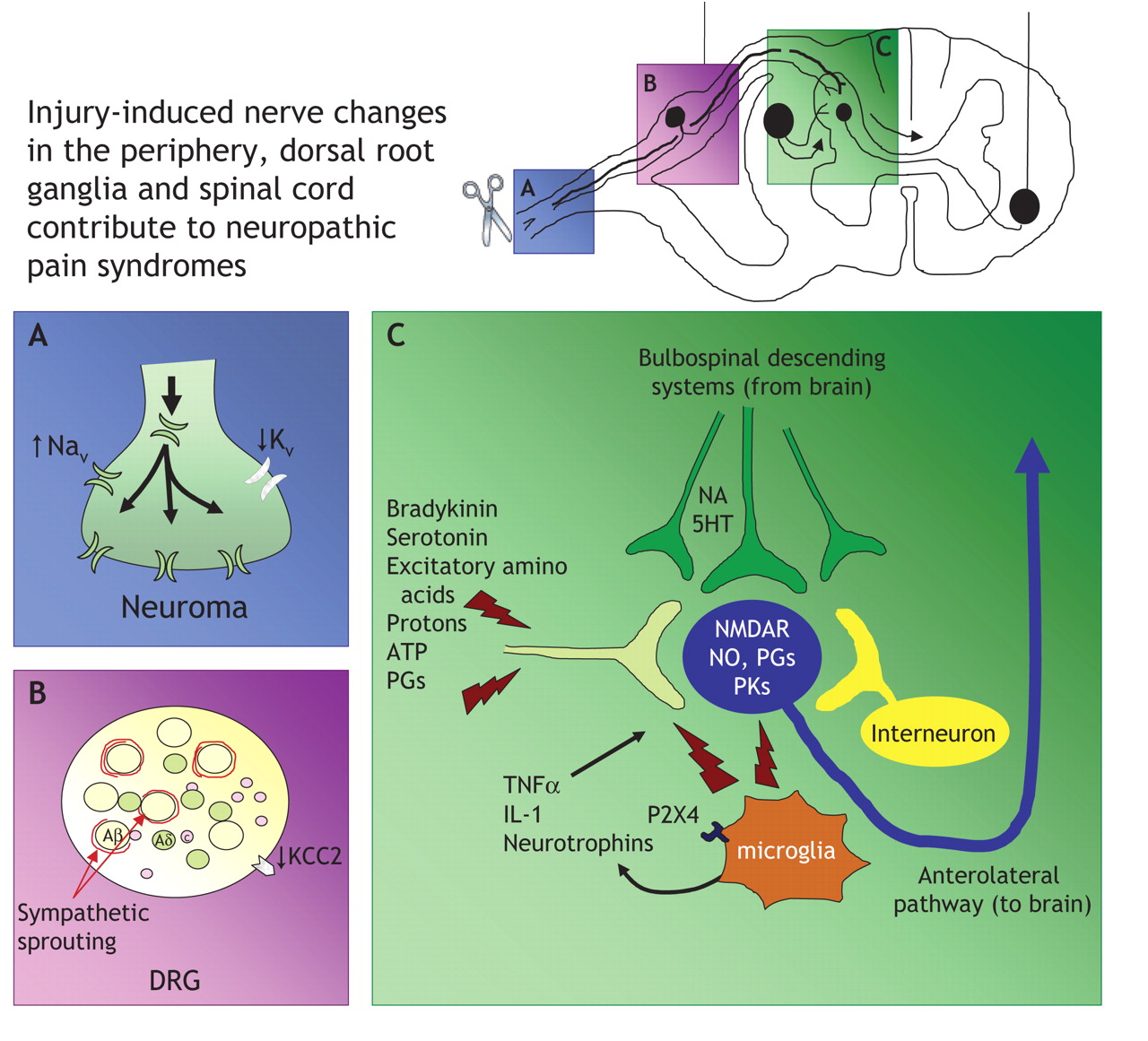
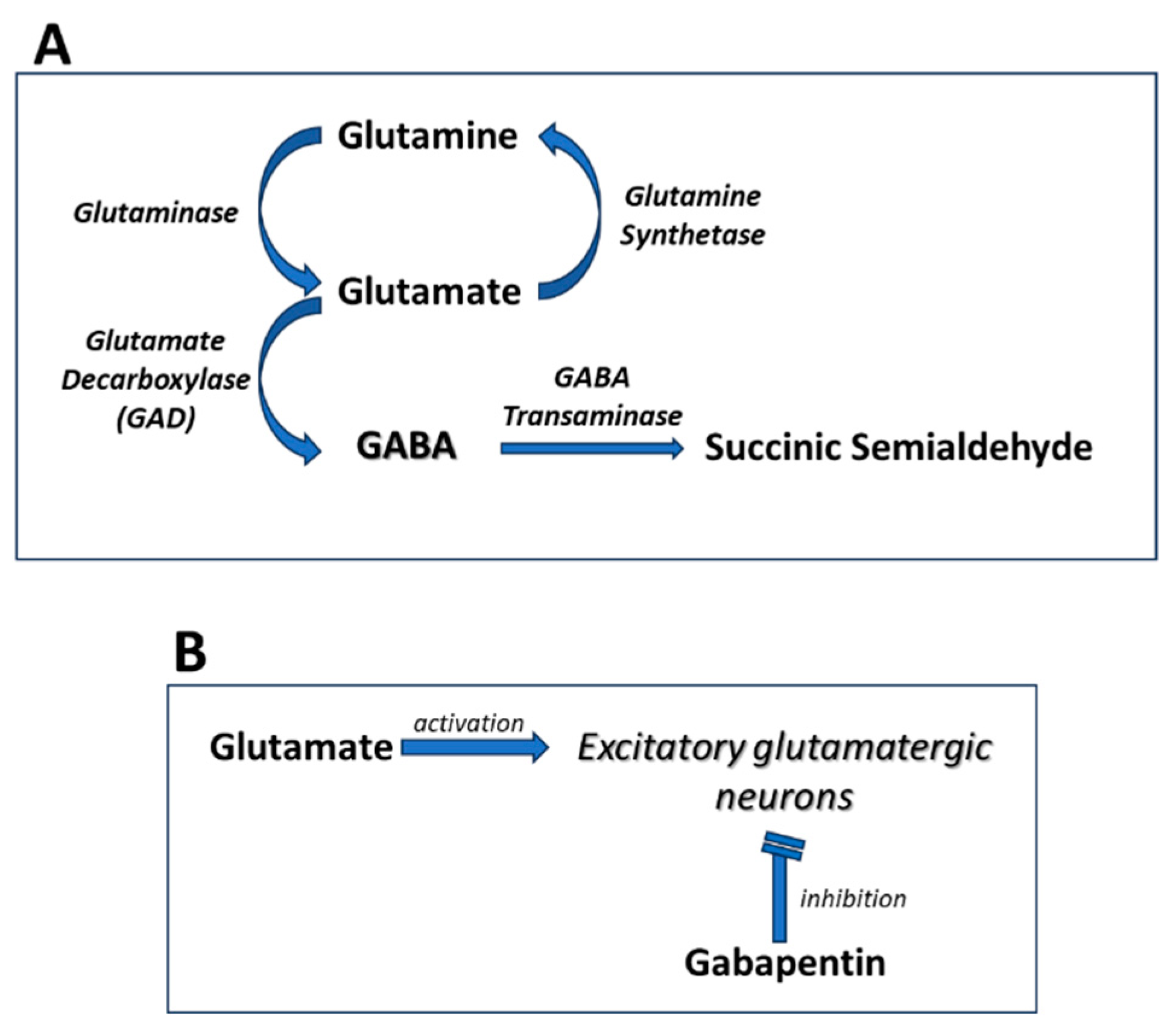
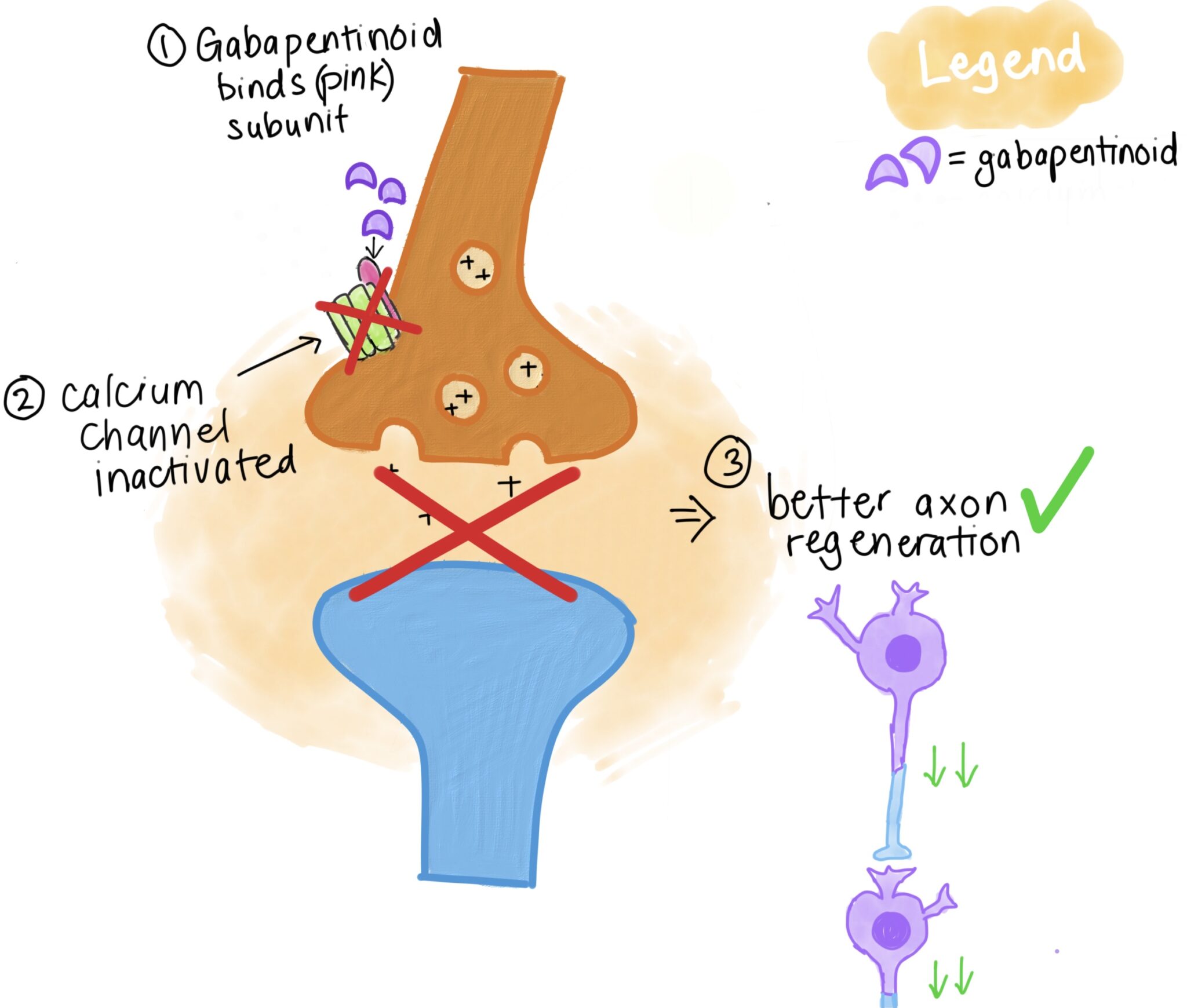
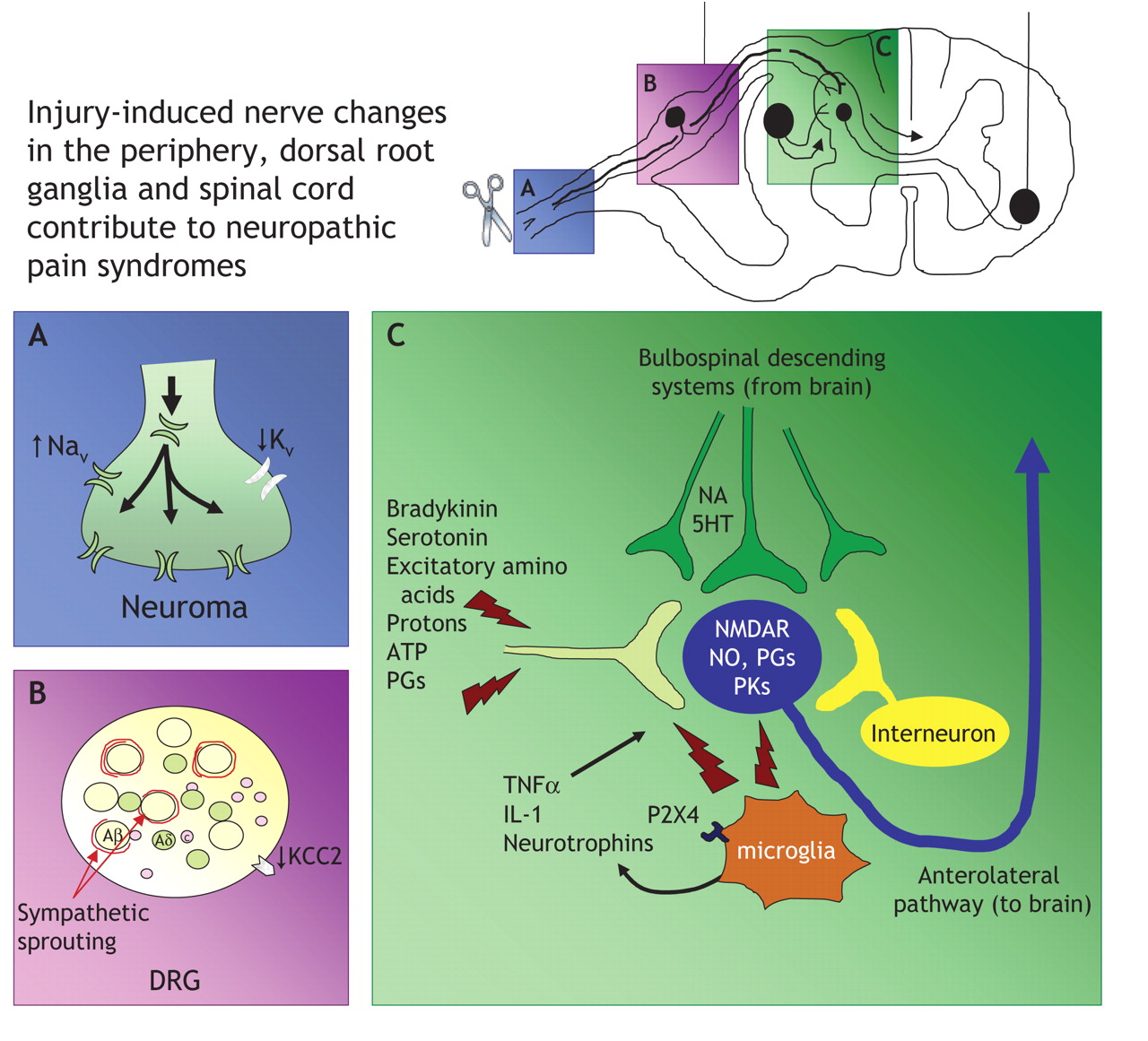
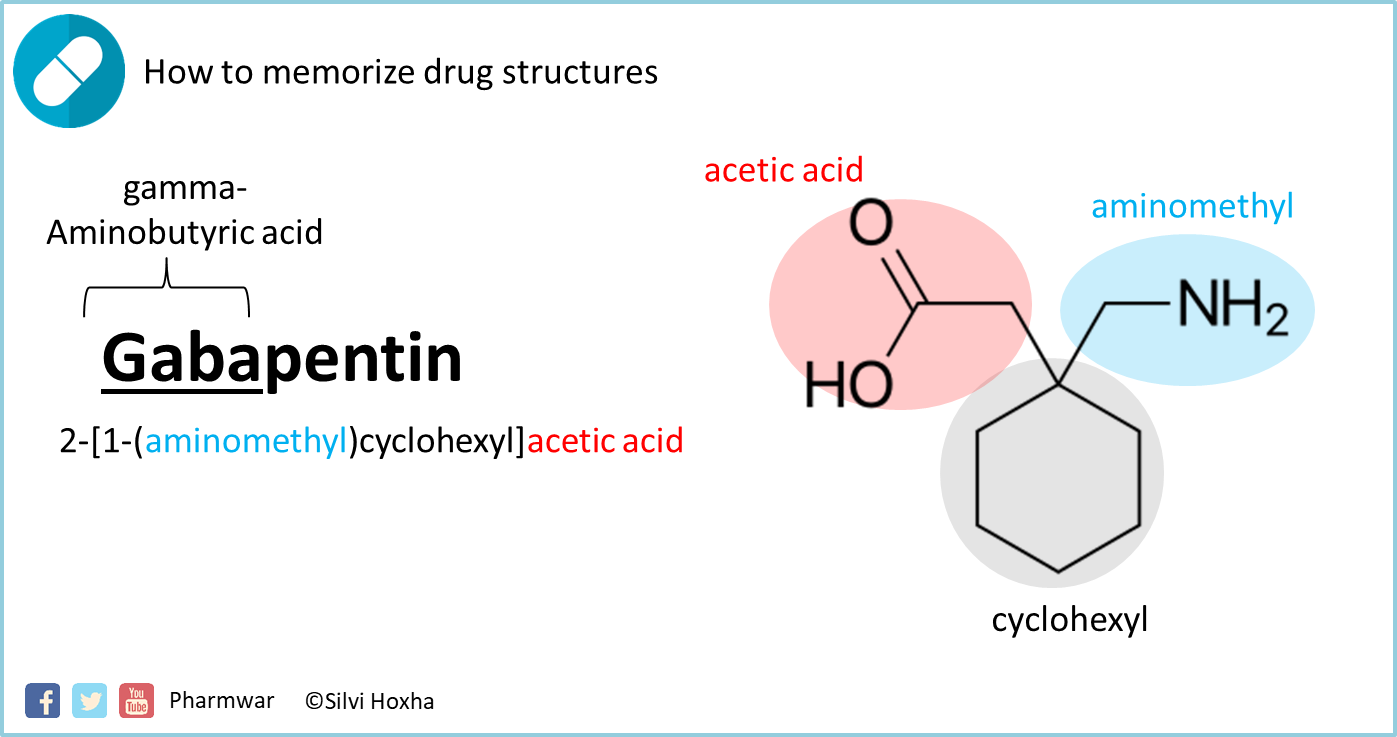
Mechanism of action. Gabapentin has no direct GABAergic action and does not block GABA uptake or metabolism. Gabapentin blocks the tonic phase of nociception induced by formalin and carrageenan, and exerts a potent inhibitory effect in neuropathic pain models of mechanical hyperalgesia and mechanical/thermal allodynia. Several mechanisms of gabapentin have been proposed after neuropathy including an inhibition of NMDA receptors, inhibition of sodium currents and reducing β4a subunit mediated VGCC trafficking (Hara and Sata 2007; Mich and Horne 2008; Yang et al. 2009). The gabapentinoid drugs gabapentin and pregabalin are antiepileptic drugs that are considered as first-line treatments for the management of neuropathic pain. 1 Pregabalin is also approved for generalised anxiety disorders in the United Kingdom. The mechanisms of action are still unclear despite their widespread use. Mechanism of Action. Although the exact mechanism of action with the GABA receptors is unknown, researchers know that gabapentin freely passes the blood-brain barrier and acts on neurotransmitters. Gabapentin has a cyclohexyl group to the structure of the neurotransmitter GABA as a chemical structure. In nerve injury models, α2δ-1 is significantly upregulated following injury and correlates with rapid gabapentin effects, while in uninjured animals/nerves, acute effects are absent or delayed. 68 In spinal nerve-injured rats, gabapentin had a significantly higher inhibitory effect on injured DRG neurons with increased N-type VGCC expression Mechanism of Action: Gabapentin modulates nerve signals to alleviate pain. Conditions Treated: Effective for neuropathic pain, fibromyalgia, and more. Dosing Guidelines: Start low and increase dosage based on individual response. Side Effects: Common effects include dizziness and fatigue; monitor closely. Comprehensive Care:Comprehensive Care: Gabapentin is an anticonvulsant medication used in the management of peripheral neuropathic pains, postherpetic neuralgia, and partial-onset seizures. The focus of perioperative pain management should be to attempt to minimise the nociceptive input and reduce the risk of transition to central sensitisation. Gabapentinoids are being increasingly used as adjuncts for management of perioperative pain. Although gabapentinoids are classed as calcium channel blockers, their mechanisms of action are poorly understood. The analgesic effect in The analgesic effect in neuropathic pain is well evidenced but the role in postoperative pain is less certain. Medline and EMBASE database searches were conducted to identify studies relating to mechanisms of action and effects in experimental animal models of inflammatory and postoperative pain and human models of experimental pain. In a meta-analysis of trials evaluating the treatment of neuropathic pain, including painful polyneuropathy and spinal cord injury pain, gabapentin was shown to be safe and effective IASP [Finnerup 2015]. Data from meta-analyses support the use of IR gabapentin for reducing pain by more than 50% in diabetic neuropathy Moore 2014, Rudroju 2013. Gabapentinoids depress neuronal excitability through interactions with the a2d-1 calcium channel subunit, stimulate descending inhibition, inhibit descending serotonergic facilitation, inhibit inflammatory media-tors, and influence the affective component of pain. Mechanism of Action. Gabapentin's exact mechanism of action is not fully understood, but it is believed to work by reducing abnormal electrical activity in the brain. It is thought to bind to calcium channels, modulating their activity and reducing the release of neurotransmitters involved in seizures and nerve pain. Gabapentin is an anti-epileptic agent but now it is also recommended as first line agent in neuropathic pain, particularly in diabetic neuropathy and post herpetic neuralgia. α2δ-1, an auxillary subunit of voltage gated calcium channels, has been documented as its main target and its specific binding to this subunit is described to produce The chemical structure of gabapentin (Neurontin) is derived by addition of a cyclohexyl group to the backbone of gamma-aminobutyric acid (GABA). Gabapentin prevents seizures in a wide variety of models in animals, including generalized tonic-clonic and partial seizures. Gabapentin has no activity at Chronic neuropathic pain is a major medical problem that remains difficult to treat. α2δ-1 (encoded by Cacna2d1) is expressed in the dorsal root ganglion (DRG) and spinal superficial dorsal horn neurons (Cole et al., 2005), and nerve injury increases α2δ-1 expression levels in both locations (Luo et al., 2001). Mechanism of action. Gabapentin has no direct GABAergic action and does not block GABA uptake or metabolism. Gabapentin blocks the tonic phase of nociception induced by formalin and carrageenan, and exerts a potent inhibitory effect in neuropathic pain models of mechanical hyperalgesia and mechanical/thermal allodynia. Its mechanisms of action appear to be a complex synergy between increased GABA synthesis, non-NMDA receptor antagonism and binding to the α, δ subunit of voltage dependent calcium channels. The latter action inhibits the release of excitatory neurotransmitters. Gabapentin is commonly used to treat neuropathic pain (pain due to nerve damage). This review updates a review published in 2014, and previous reviews published in 2011, 2005 and 2000. To assess the analgesic efficacy and adverse effects of Gabapentin has become popular as a first-line treatment for neuropathic pain because of its efficacy as an antineuropathic agent and relatively benign side-effect profile. However, its In randomized open clinical trial, the combination of gabapentin with opioid analgesics was shown to provide better relief in neuropathic pain in cancer patients as compared to opioid analgesics alone in terms of reduction in pain intensity for burning and shooting pain at different days of the study.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |